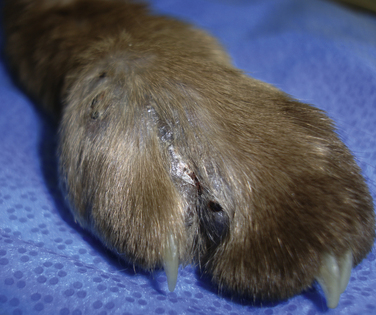
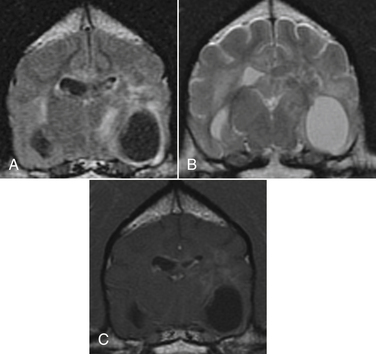
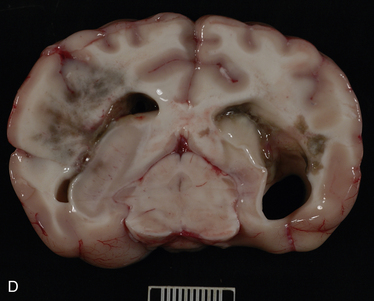
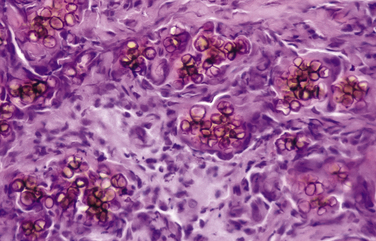
Chapter 68 Unlike the common endemic fungal pathogens (for which a definitive diagnosis can often be made simply by visualizing the unique morphologic features of the organism in cytologic or histologic samples), opportunistic fungi can only be identified to genus and species level by culture or molecular methods. However, they can be assigned to categories based on their morphologic features in tissue, such as pigmentation, hyphal diameter, and frequency of septation. These categories include phaeohyphomycosis (pigmented hyphal or yeast forms), hyalohyphomycosis (nonpigmented hyphal forms), eumycotic mycetoma (fibrosing granuloma with black or white tissue grains consisting of aggregates of pigmented or nonpigmented fungi, respectively), and zygomycosis (wide, infrequently septate, nonpigmented hyphae associated with pyogranulomatous and eosinophilic inflammation). Because of its similarities to pythiosis and lagenidiosis, zygomycosis is discussed in Chapter 69. Although identification of a specific pathogen after culture is ideal, classification of opportunistic mycoses based on the categories just listed is usually sufficient to allow the clinician to make a reasonable prediction about clinical course and prognosis and to make appropriate treatment decisions. Because many opportunistic fungi are common contaminants and can normally be found on skin, nasal mucosa, and other nonsterile sites, culture- or PCR-based identification of a potential opportunistic fungal pathogen from a skin specimen, nasal swab, or exudate should not be considered evidence of fungal infection unless there is supportive histologic or cytologic evidence of tissue invasion by a morphologically compatible organism. The term “phaeohyphomycosis” refers to cutaneous, subcutaneous, cerebral, or disseminated infections caused by pigmented (also known as dematiaceous) fungi that contain melanin in their cell walls.1 Infection usually results from cutaneous inoculation. Fungal genera that have been identified as agents of phaeohyphomycosis in veterinary patients include Alternaria, Bipolaris, Cladophialophora, Curvularia, Exophiala, Fonsecaea, Moniliella, Phialophora, Ramichloridium, Ulocladium, and Scolecobasidium, among others (Table 68-1). TABLE 68-1 Causative Agents and Histologic/Cytologic Characteristics Associated with Miscellaneous Fungal and Pseudofungal Pathogens The most common clinical manifestations of phaeohyphomycosis in immunocompetent small animals are lesions associated with the digits, pinnae, nasal planum, or nasal cavity in cats (Figure 68-1). 2–8 Cutaneous lesions occur less often in dogs.9 In addition, granulomatous meningoencephalitis caused by pigmented fungi (especially Cladophialophora bantiana) have been described both in dogs and cats.10–14 In immunocompromised patients, the most common presentation appears to be multifocal cutaneous lesions in dogs treated with multiagent immunosuppressive therapy, especially that which includes cyclosporine.15–17 FIGURE 68-1 Left distal thoracic limb of an 8-year-old male neutered Burmese cat with digital phaeohyphomycosis. (Courtesy University of California, Davis, Veterinary Dermatology Service.) Animals with phaeohyphomycosis typically have cutaneous nodules or a visible nasal mass. Infected tissues may appear grossly pigmented, and thus masses may be confused with melanomas. Phaeohyphomycoses tend to be locally invasive and may extend to involve regional lymph nodes (Figure 68-2). Systemic dissemination more often occurs in animals treated with immunosuppressive drugs, but disseminated infections have also been described in apparently immunocompetent patients.18,19 Animals with central nervous system (CNS) phaeohyphomycosis may have neurologic signs such as obtundation, seizures, abnormal placing reactions, circling, tremors, ataxia, and abnormal cranial nerve function. Laboratory and Imaging Abnormalities Results of a CBC, biochemistry panel, and urinalysis in animals with cutaneous phaeohyphomycoses are typically unremarkable. Animals with disseminated disease can have abnormalities associated with underlying immunosuppressive illness or drug treatment. Imaging with computed tomography (CT) or MRI in animals with CNS involvement may reveal focal or multifocal contrast-enhancing lesions that may be associated with hydrocephalus (Figure 68-3). FIGURE 68-3 Axial T1 postcontrast, T2, and FLAIR magnetic resonance images (A, B, and C, respectively) of the brain of a 6-year-old male neutered Border collie mix that was evaluated for neurologic signs including seizures and progressive obtundation. In the images shown, there is bilateral but asymmetric ventricular dilation that is severe on the right and mild to moderate on the left (asymmetric hydrocephalus). Multifocal regions of contrast enhancement are also present (A). Some of these regions appeared nodular; others had a ring-like appearance. There is also marked contrast enhancement of the ventricular ependymal lining. The regions of contrast enhancement correlate with regions of T2 and FLAIR hyperintensity (B and C) and were isointense on precontrast T1-weighted sequences (not shown). Meningoencephalitis caused by Cladophialophora bantiana and secondary hydrocephalus was diagnosed on brain biopsy and at necropsy (D). Olive-green pigmented masses can be seen on both the left and right sides of the brain. Interestingly, the dog also had cutaneous protothecosis. (Courtesy University of California, Davis, Veterinary Neurology and Anatomic Pathology Services.) On histologic or cytologic examination, fungi that cause phaeohyphomycosis appear as dark-walled, irregularly septate hyphae or as yeast-like cells, solitary or in small groups or chains (Figure 68-4). Pigmentation may not always be apparent on cytologic examination (Figure 68-5). The presence of melanin in the walls of lightly-pigmented hyphae can be confirmed by the examination of unstained sections, by lowering the microscope condenser during examination, or by utilization of a Fontana-Masson stain for melanin. FIGURE 68-4 Histopathology showing small groups of pigmented, yeast-like fungal organisms in tissue from a nasal mass in a cat with phaeohyphomycosis; H&E stain. (Courtesy Amy Grooters, Louisiana State University, Baton Rouge, LA.) FIGURE 68-5 Impression smear from the brain of the dog in Figure 68-3.
Miscellaneous Fungal Diseases
Phaeohyphomycosis
Disease
Causative Agents
Histologic and Cytologic Characteristics
Phaeohyphomycosis
Alternaria, Bipolaris, Phialophora, Cladophialophora (Cladosporium), Curvularia, Exophiala, Fonsecaea, Moniliella, Ochroconis, Ramichloridium, others
Pyogranulomatous inflammation associated with pigmented, irregularly septate hyphae or yeast-like cells that may be solitary or may cluster in small groups or chains
Hyalohyphomycosis
Acremonium, Fusarium, Geotrichum, Geosmithia, Paecilomyces, Phialosimplex, Pseudallescheria, Sagenomella, Scedosporium, Schizophyllum, others
Pyogranulomatous inflammation associated with hyphal elements that have nonpigmented (transparent, hyaline) walls; Phialosimplex may cause yeast-like forms in tissue
Mycetoma
(black-grain)
Curvularia
Pyogranulomatous inflammation associated with aggregates of pigmented fungal organisms (which appear grossly as pigmented tissue grains)
Mycetoma
(white-grain)
Pseudallescheria boydii, Acremonium
Pyogranulomatous inflammation associated with aggregates of nonpigmented fungal organisms (which appear grossly as nonpigmented tissue grains)
Pythiosis
Pythium insidiosum
Pyogranulomatous and eosinophilic inflammation associated with broad (2-7 µm), infrequently septate hyphae (see Chapter 69)
Lagenidiosis
Lagenidium
Pyogranulomatous and eosinophilic inflammation associated with broad (4-25 µm), infrequently septate hyphae (see Chapter 69)
Zygomycosis
Conidiobolus spp., Basidiobolus ranarum in dogs; Rhizomucor, Mucor, and Cokeromyces in cats
Pyogranulomatous and eosinophilic inflammation associated with broad (5-20 µm), infrequently septate hyphae with thick prominent eosinophilic sleeve (see Chapter 69)
Aspergillosis
Aspergillus terreus, A. deflectus, A. flavipes, A. fumigatus, others
Suppurative to granulomatous inflammation associated with multiple, nonpigmented, 3- to 6-µm, septate hyphae with parallel walls and 45-degree angle branching (see Chapter 65)
Candidiasis
Candida albicans, other Candida spp.
Suppurative inflammation with numerous 2- to 6-µm oval yeasts, pseudohyphae (chains of oval yeast cells), and true hyphae (see Chapter 67)
Clinical Features
Diagnosis
Cytologic and Histologic Findings
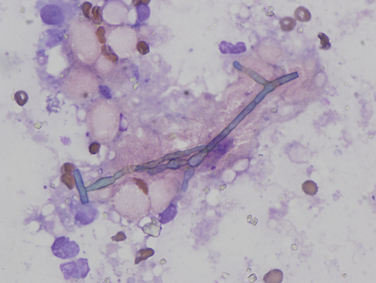
Septate, branching hyphae are present, but pigmentation is not clearly apparent. Wright’s stain, 1000× magnification. (Courtesy University of California, Davis, Veterinary Pathology Service.)![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Miscellaneous Fungal Diseases
Only gold members can continue reading. Log In or Register to continue

