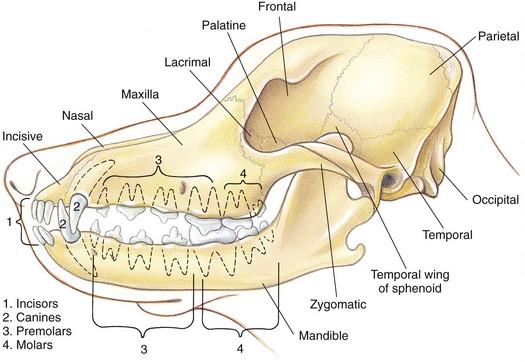
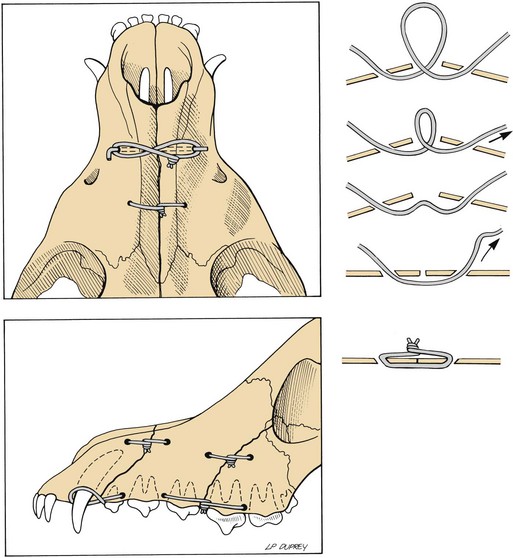
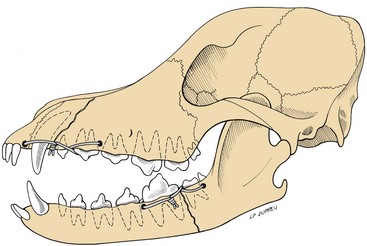
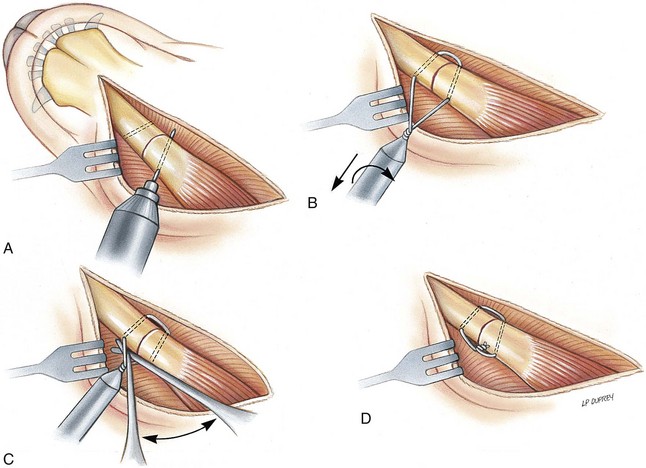
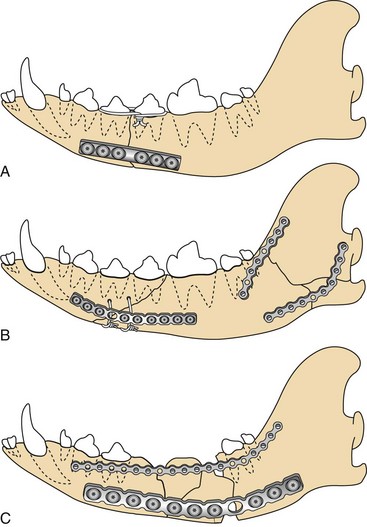
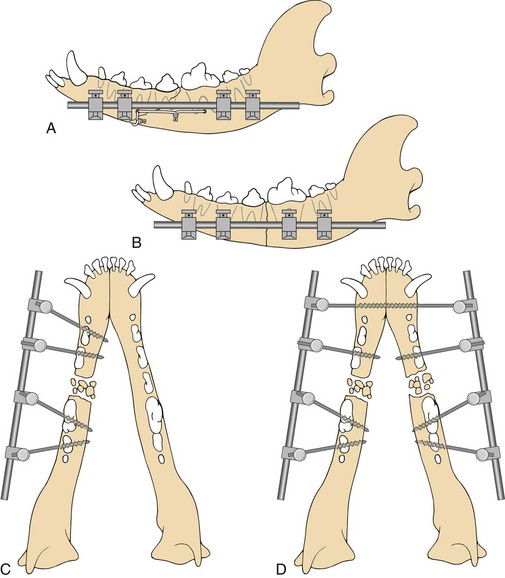
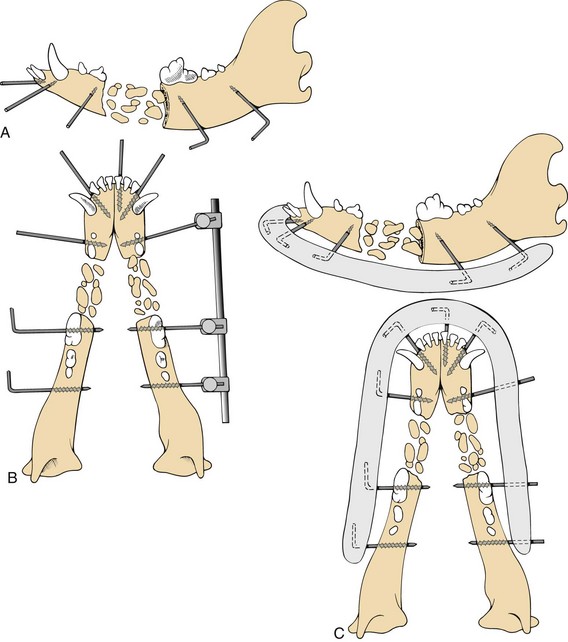
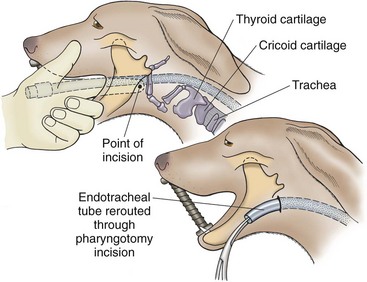
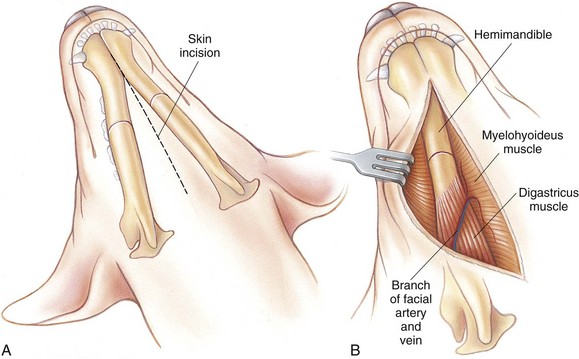
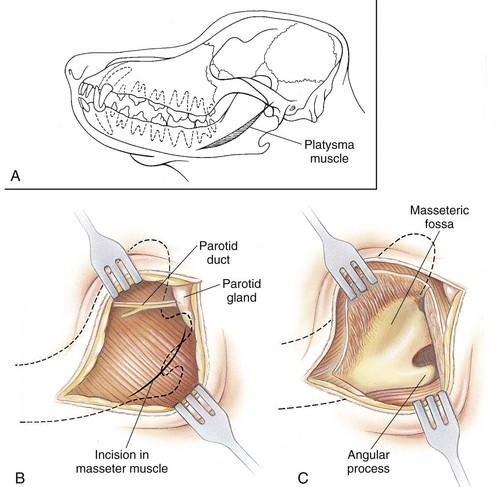
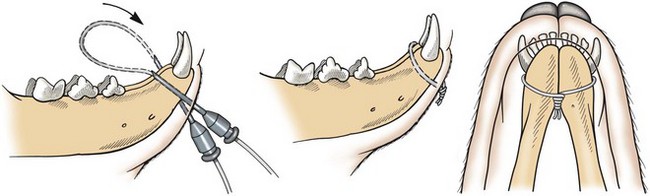
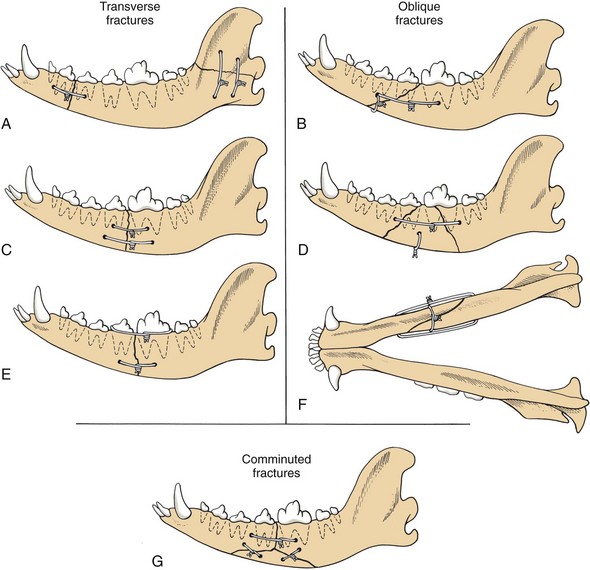
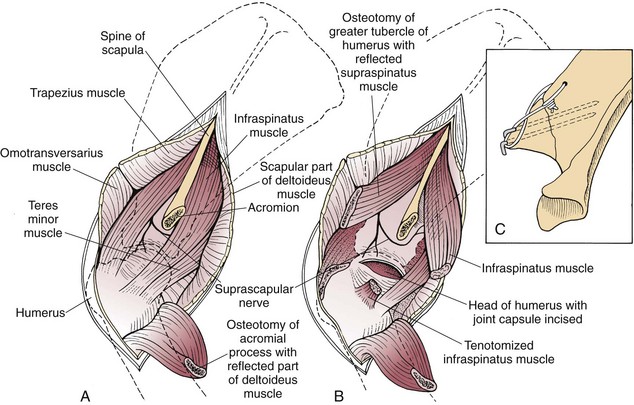
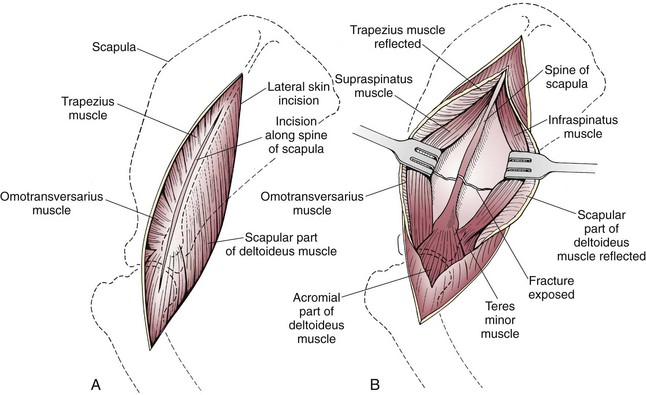
Chapter 33 Maxillary and Mandibular Fractures Maxillary and mandibular fractures are usually caused by head trauma, and concurrent injuries (i.e., upper airway obstruction, central nervous system trauma, pneumothorax, pulmonary contusions, and traumatic myocarditis) are often present. These abnormalities may be acutely life-threatening and may require prompt diagnosis and treatment. Definitive fracture repair often must be delayed until the animal has been appropriately stabilized. Mandibular fractures occasionally occur as a result of bone loss associated with severe periodontitis. Teeth extraction should be performed with care in older patients with severe periodontitis to prevent this complication. With severe periodontitis, bone healing may be impaired. Diseased teeth must be extracted before fracture stabilization in these patients. Pathologic fractures may also result from mandibular neoplasia (see p. 412). Histopathologic examination of bone from animals with mandibular fractures is warranted, unless fractures clearly are caused by trauma. Mandibular fractures associated with neoplasia are treated by mandibulectomy rather than by definitive fracture repair (see p. 412). The teeth occupy a large portion of the mandible and are integral components of normal mandibular structure (Fig. 33-1). Teeth involved in fractures should not be removed unless they are loose. This is especially important with fractures involving the caudal mandibular body because the large premolar and molar teeth occupy a substantial portion of this bone and are essential contributors to fracture stability. Fractures extending along the tooth root from the alveolar crest to the apex of the tooth are at risk for pulpal necrosis and periapical bone resorption. Temporary or permanent root canal therapy at the time of fracture stabilization may promote bone healing. If affected teeth are not treated at surgery, periodic evaluation for evidence of infection or loosening is necessary postoperatively to determine whether endodontic therapy or extraction is indicated. The anatomy and location of tooth roots must be considered when implants are applied to the mandible. Damage to tooth roots from pins, wires, drill bits, and screws may cause sufficient damage that extraction becomes necessary after fracture healing. Radiographs of the mandible and maxilla generally require that animals be anesthetized. Thorough radiographic examination of the skull usually requires a minimum of four radiographic views: dorsoventral or ventrodorsal, lateral, and right and left lateral obliques. Skull radiographs are often difficult to interpret because of the presence of multiple overlying structures; therefore comparison with a normal skull is often helpful. Symmetry between the two sides is critical to interpretation, thus care in positioning is critical. Additional specialized views, such as intraoral views, may be necessary for complete evaluation. Computed tomography (CT) can help identify fractures in the caudal mandibular body, vertical ramus, and mandibular condyle that may be difficult to detect radiographically. CT is often more efficient than survey radiography for evaluating complex mandibular and maxillary fractures (Bar-Am et al, 2008). A tape muzzle may be applied to support the mandible if minimal displacement of fracture fragments (usually fractures of the ramus) occurs, if dental occlusion is adequate, and if the fracture assessment score (see p. 1055) is favorable and dictates early union. A muzzle can be made from two pieces of tape placed with the sticky sides together and fashioned into a circle that fits over the dog’s nose. A similarly made piece of tape extends from the circle around the head and behind the ears (Fig. 33-2). The muzzle should allow the dog to open its mouth enough to lap water and eat gruel. To allow adequate healing, muzzles should remain in place for 6 weeks. Dogs with mandibular plus maxillary fractures may not tolerate tape muzzles because the muzzle may put pressure on the maxillary fracture. Because of the cat’s short nose, tape muzzles are difficult to apply and maintain. Similarly, it may be difficult to maintain a tape muzzle in brachycephalic breeds. The crowns of the mandibular teeth are cleaned, pumiced, and acid-etched to improve acrylic resin bonding. The mandible is aligned using interdigitation of the teeth as a landmark for accurate reduction. Interdental wire ligatures (0.3 to 0.5 mm wire) are applied to initially stabilize the fracture(s). Dental acrylic is applied to the prepared teeth to stabilize the fracture (Fig. 33-3). The splints are removed when radiographic evidence reveals bone bridging the fracture by sectioning the splint interdentally and removing the splint in sections. Bonding the maxillary and mandibular canine teeth together in anatomic alignment is an alternative to the tape muzzle for conservative fracture treatment. The canine teeth are cleaned, pumiced, acid-etched, and aligned with dental composite, leaving the mouth open approximately 1 cm. Although simple, the technique requires that all four canine teeth be intact and healthy. This technique can be used in dogs and cats (Fig. 33-4). The appropriate method of treating mandibular and maxillary fractures is determined on the basis of the fracture assessment score (see p. 1055) and fracture location. Conservative treatment with a tape muzzle or dental composite bonding may be appropriate for some fractures (see previous discussion). Internal fixation systems applicable for mandibular fractures include orthopedic wire, Kirschner wire, and plates and screws. Intramedullary (IM) pins are contraindicated because the mandibular canal contains the mandibular alveolar artery and the inferior alveolar nerve. External fixators (both standard and acrylic frames) are very effective for nonreducible comminuted fractures. Many maxillary fractures are nondisplaced and require only conservative therapy; however, segmental maxillary fractures or depressed fracture lines may require repositioning and stabilization. Mandibular or maxillary fractures that alter normal occlusion should be reduced and stabilized. Maxillary fractures that result in nasal malpositioning or instability should be reduced and stabilized. Interfragmentary wires may be used to stabilize some maxillary fractures where only a few large bone fragments are involved and stable anatomic reduction is possible (Fig. 33-5), especially with Kirschner wires incorporated into the fixation to prevent overriding of the fragments. Maxillofacial miniplates are more effective for restoring anatomic contour to comminuted and depressed maxillary fractures involving thin portions of the skull. Interdental wires are placed around teeth adjacent to fracture lines. Position the wires securely in the bone around the tooth’s neck to prevent them from sliding off the crown. Place the wires through guide holes that are drilled between the teeth and through the superficial cortical bone surface. Pass the wire through the guide holes, circling the teeth, and tighten. Bend the ends of the wire into the mucosa (Fig. 33-6). Interfragmentary wires are ideal for stabilizing relatively simple, reconstructible mandibular and maxillary fractures. Large-gauge wire (18 to 22 gauge), properly applied, provides adequate fracture support (Table 33-1); however, wires may be difficult to position and tighten unless certain application guidelines are followed. The largest gauge wire that can be manipulated should be used. Use Kirschner wires to drill holes in the bone, 5 to 10 mm from the fracture line (Fig. 33-7, A). Position these holes so that the wire will be perpendicular to the fracture line when it is tightened. Slope the drill holes toward the fracture line because this results in obtuse angles on the bone side opposite to where the wire knot will be tightened. This positioning allows the wire to slide into position easily and enhances tightening efforts. Use long segments of wire to facilitate wire passage and allow manipulation of any wire kinks away from the area of wire that is to be tightened. Tighten the wire using a twist knot or a tension loop (see p. 1086). Twist it in such a manner that equal tension is applied to both strands (Fig. 33-7, B). Use a periosteal elevator or large tissue forceps to lever the orthopedic wire under the twist and eliminate slack (Fig. 33-7, C). When tightened, bend the wire perpendicular to the wire surface and away from the gingival margin. Cut the wire and twist the ends and bend them into the bone surface (Fig. 33-7, D). Optimally, wires should be located near the oral margin to neutralize forces that tend to disrupt fractures. Because this margin also contains the teeth, care must be used to position drill holes between teeth or tooth roots. When multiple wires are used, all holes should be drilled and wires positioned before any wires are tightened. Wires are tightened beginning at the caudal fracture line and working toward the symphysis. If bending or slippage is encountered with oblique or transverse fractures, Kirschner wires with figure-8–patterned orthopedic wire may be used. The Kirschner wire helps prevent sliding or bending while the orthopedic wire is tightened. Comparable Wire Sizes for Fracture Stabilization Bone plates can be used to stabilize single or comminuted mandibular fractures (see p. 1086). Plates are applied to the ventrolateral mandibular surface. Care must be used to contour the plate correctly because the mandible aligns with the plate as the screws are tightened; malalignment results in malocclusion. Screws are positioned to avoid tooth roots. Maxillofacial miniplates may offer easier contouring and screw placement in mandibular and maxillary fractures and may be combined with standard straight plates and reconstruction plates (Fig. 33-8). External fixators (see p. 1067) can be used to stabilize mandibular body fractures if sufficient bone is present to hold fixation pins. Fixation pins are placed percutaneously through the mandibular body, avoiding tooth roots. Type I fixators are applied to the ventrolateral mandibular surface with at least two pins inserted on either side of the fracture line. Positive-profile, end-threaded pins are used to increase the fixator’s holding power. For bilateral mandibular body fractures, a type II fixator may be constructed using bilateral and unilateral fixation pins. A connecting bar is placed on either side of the dog’s jaw (Fig. 33-9). Dental acrylic, used to replace clamps and connecting bars, is a versatile rigid fixation for mandibular fractures, especially severely comminuted fractures. After pins have been placed in appropriate locations in the mandible (use fixation pins of appropriate size for the bone area), the ends are bent parallel to the skin (Fig. 33-10, A). To evaluate dental occlusion and reduce fractures, the animal’s mouth is closed. If necessary, Kirschner clamps and a connecting bar can be placed to hold the fracture temporarily in reduction while the acrylic is being mixed and molded (Fig. 33-10, B). Soft tissue is protected by laying wet sponges beneath the pins. After the acrylic is mixed, it is molded over the bent pins to form a connecting bar (Fig. 33-10, C). Alternatively, plastic tubing may be impaled over the pins (do not bend them) and then used as a mold for the liquid-phase acrylic. The acrylic splint can be curved around the rostral portion of the mandible. Animals with mandibular fractures that have high fracture assessment scores of 8 to 10 (e.g., simple fractures in young animals; see p. 1055) may be treated with tape muzzles, interdental fixation, interdental wiring, or interfragmentary wiring techniques, depending on fracture location. Interfragmentary wire is usually sufficient to stabilize simple, bilateral, mandibular fractures if they can be anatomically reconstructed, and if fracture assessment scores indicate rapid healing (Box 33-1). It has the advantage of providing internal fixation with minimal aftercare. With moderate fracture assessment scores of 4 to 7 (e.g., larger or older dogs with longer healing times) and if bilateral fractures can be anatomically reconstructed, interfragmentary wires, interdental fixation, external fixation, or bone plates and screws may be used for fracture fixation. A cancellous bone autograft can be used to promote rapid bone union in these patients. With low fracture assessment scores of 0 to 3 and comminution, bone loss, or severe soft tissue damage, mandibular fractures are best treated with closed reduction and external fixator application or bridging plate application. Closed reduction techniques preserve the biological environment, but external fixators require intensive aftercare, and the pin-bone interface loosens over time. Mandibular alignment is determined by observing dental occlusion. Plate and screw fixation can be used to stabilize mandibular fractures with cortical bone loss; however, the plate must be carefully contoured to the normal shape of the fractured bone. If open reduction is performed in patients with low fracture assessment scores, autogenous cancellous bone or demineralized bone matrix with cancellous bone allograft can be used to facilitate healing. After the status of the animal has been determined, mandibular fractures in most dogs may be gently reduced and temporarily held in position with a tape muzzle until a definitive stabilizing procedure can be performed (see Fig. 33-2). However, mandibular fractures in cats and brachycephalic dogs cannot be easily stabilized with tape muzzles and often are not treated until surgery. Because the oral cavity contains numerous bacteria, prophylactic antibiotics are recommended. Infections are rare, however, because the vasculature supplying this area is well developed and plentiful. If infection is likely and if open reduction is performed, bacterial cultures can be submitted during surgery. Analgesics should be provided to posttraumatic animals (see Chapter 12). Anatomic reconstruction or realignment of mandibular cortices is mandatory to provide proper dental occlusion. Simple mandibular fractures can be anatomically reconstructed using bone cortex as a guide. With complex fractures or cortical bone loss, however, dental occlusion must be used to guide mandibular realignment. Because mandibular and maxillary teeth closely interdigitate, precise alignment of upper and lower arcades is necessary. If precise dental occlusion cannot be determined with the endotracheal tube in place, it may be repositioned through a pharyngotomy incision (Fig. 33-11). This allows the mouth to be completely closed during surgery, which facilitates determination of adequate dental occlusion. After surgery, the endotracheal tube is removed, and the pharyngotomy incision is allowed to granulate closed. Another anesthetic technique involves intermittently extubating and reintubating the patient to allow the surgeon an opportunity to check alignment. This technique requires careful patient selection. Patients with compromised pulmonary or cardiac function may not handle even short periods of extubation. It is important that the patient be relatively easy to rapidly intubate. Furthermore, some complicated fractures may not lend themselves to such a technique, and pharyngostomy should be planned. For an intermittent ventilation technique to work, it is necessary for the surgeon and the anesthetist to be in constant communication. Before extubation, the patient should be receiving 100% oxygen and vital signs should be within the normal range. A pulse oximetry reading of 100% at extubation usually allows the surgeon several minutes to check occlusions and make adjustments. When pulse oximetry begins to drop into the low 90’s, the anesthesia provider needs to reintubate and ventilate with 100% oxygen. If necessary, this can be repeated several times as long as the patient’s oxygenation remains adequate and the vital signs remain normal. Intermittent small boluses of a short-acting hypnotic such as propofol may be necessary when the patient is not receiving an inhalational agent (see Tables 32-5 and 32-6 on pp. 1045-1048). Bones of the maxilla and mandibular body are easily palpated and surgically approached through skin and subcutaneous tissue (Fig. 33-12). The maxillary nerve (branch of the trigeminal nerve that innervates cutaneous muscles of the head, nasal and oral cavities, and muscles of mastication) passes rostrally through the alar canal and can be injured by maxillary fracture. The mandibular alveolar nerve, which is sensory to the teeth of the mandible, passes through the mandibular canal along with the mandibular alveolar artery. These structures are frequently damaged by mandibular fracture, although clinical signs are seldom evident. Tooth roots must be avoided when implants are placed in the maxilla or mandible. The approach to the ramus and the temporomandibular joint involves dissection and elevation of the masseter muscle (Fig. 33-13). The parotid duct and gland and the facial nerve are dorsal and superficial to the masseter muscle and should be avoided. Open Reduction of Mandibular Fractures With bilateral mandibular fractures, make a ventral midline incision in the skin between the mandibles. Move this incision in either direction to expose both mandibles. If only one mandible is involved, make a ventral skin incision directly over that mandible. Elevate soft tissue from the mandibles to expose the fracture(s). Maintain the digastricus muscle attachment (see Fig. 33-12). Reduce and stabilize the fracture (see p. 1116). If a segmental fracture of the mandibular body occurs, stabilize the caudal fracture first. Because little musculature is present around the mandibular body, reduction usually is easily accomplished. Open reduction of the mandibular cortex will realign the teeth. Evaluate the oral cavity for open wounds. If large wounds are present, close the mucosa partially to decrease their size. To allow postoperative drainage, do not completely close contaminated wounds. Place a Penrose drain if infection is present or likely. Close the surgical wound by suturing apposing layers. Make a skin incision over the ventrolateral border of the caudal mandibular body, and separate the platysma muscle to expose the digastricus muscle. Elevate the masseter muscle from the ramus to expose its lateral mandibular surface and angular and coronoid processes (see Fig. 33-13). Reduce the fracture and stabilize it (see p. 1115). Repair large, open wounds of the oral cavity as described on p. 1115. Close the surgical wound by suturing apposing layers. Make a skin incision over the fracture(s), and gently elevate the soft tissue from the bone. Reduce the fracture and stabilize it. Repair large, open wounds to the oral cavity as described on p. 1115. Symphyseal fractures are best treated with cerclage wire. A single wire serves as effective treatment for symphyseal fractures. Symphyseal cerclage wires encircle the mandible caudal to the canine teeth. The wire can be removed once the fracture has healed (generally 6 to 8 weeks) by cutting it with wire scissors where it is exposed behind the canine teeth. Make a small nick in the skin overlying the ventral aspect of the symphysis. Insert a 16 g or 18 g hypodermic needle through this nick and along one lateral mandibular surface (under the subcutaneous tissue). Exit the needle in the oral cavity caudal to the canine tooth, and thread an 18 g or 20 g wire through the needle. Reposition the needle on the opposite side of the mandible, curve the wire across and behind the canine teeth, and reinsert it through the hypodermic needle. Exit the wire from the skin incision at the original insertion point. Once the fracture is reduced, tighten the wire. Leave the ends of the wire exposed through the skin incision, and bend them to decrease the possibility of injury to the owner (Fig. 33-14). Transverse fractures should be realigned and compressed. Apply one or two interfragmentary wires perpendicular to the fracture line to achieve compression (Fig. 33-15, A to C). Alternatively, if the patient’s fracture warrants more rigid fixation, use an external fixator or compression bone plate. Oblique fractures may override when parallel wires are tightened so that alternative wire patterns may be required. Stabilize caudal to rostral (or vice versa) oblique fracture lines with two wires placed at right angles to each other. More than one wire may be placed through a single drill hole. Stabilize medial to lateral (or vice versa) oblique fracture lines with two wires placed perpendicular to each other in two perpendicular planes. In both cases, the second wire prevents overriding of the fracture as the wires are tightened (Fig. 33-15, D to F). Stabilize comminuted fractures that have long fracture lines and can be anatomically reconstructed with interfragmentary wires (Fig. 33-15, G). Support the reconstructed fracture with a bone plate or external fixator. Bridge comminuted fractures that cannot be reconstructed with a bone plate or external fixator. Pay careful attention to ensure that dental occlusion is appropriate. Postoperative radiographs should be evaluated for implant position. Occlusion of the teeth, however, takes precedence over accurate fragment reduction. Dental occlusion is more readily determined by physical examination than with radiographs. Occasionally a tape muzzle can be used postoperatively to support the fixation (see Fig. 33-2). When muzzles are used as primary fixation or support for internal fixation, the skin on the ventral surface of the mandible may become irritated. The skin should be carefully cleaned and treated with a soothing ointment. External fixators should be evaluated postoperatively to ensure that the clamps or acrylic is not too close to the skin. The animal should be fed soft food until the fracture heals; chew toys should be avoided. Patients with maxillomandibular fixation who have difficulty with oral feeding may benefit from an esophageal feeding tube (see p. 102). Owners should be instructed to not allow the animal to chew on rocks or sticks or to play tug-of-war. Clients should be instructed to clean the skin beneath a tape muzzle daily and to clean the area around external fixation pins. Oral chlorhexidine rinses twice daily are recommended for patients with interdental splints to minimize gingivitis associated with entrapped debris. The animal should be re-evaluated 2 weeks postoperatively and sutures removed. Radiographs should be obtained after 6 weeks to evaluate healing and repeated every 6 weeks thereafter until healing is complete. Dental composite used for tooth bonding may break prematurely and require reapplication if healing is not complete. Dental composite, intraoral wires, and external fixators should be removed when fractures are healed; interfragmentary wires and bone plates and screws are not removed unless they cause problems. Sectioning the interdental splint and removing it segmentally helps avoid fracturing of teeth during this maneuver. Common complications include malocclusion and osteomyelitis. Many animals learn to compensate for malocclusion; however, temporomandibular arthritis, impaired mastication, abnormal tooth wear, plaque and tartar accumulation, and periodontitis are possible sequelae. Mild malocclusion associated with interference of teeth can be treated by remodeling the involved teeth to allow clearance. Severe malocclusion may require tooth extraction or corrective osteotomy. Osteomyelitis (see p. 1407) and bone sequestration should be treated by sequestrectomy, removal of loose implants, mandibular stabilization (if necessary), cancellous bone autografts, culture/sensitivity, and appropriate antibiotics. Nonunions are treated with appropriate stabilization and cancellous bone autografts. Partial mandibulectomy (see p. 392) is an option for treatment of chronic nonunion of the mandible. Beckman, B, Smith, MM. Interarcade bonding for non-invasive mandibular fracture repair. J Vet Dent. 2009;26:62. Bennett, JW, Kapatkin, AS, Manfra-Marretta, S. Dental composite for the fixation of mandibular fractures and luxations in 11 cats and six dogs. Vet Surg. 1994;23:190. Boudrieau, RJ. Fractures of the maxilla. In: Johnson AL, Houlton JEF, Vannini R, eds. AO principles of fracture management in the dog and cat. Thieme, NY: AO Publishing, 2005. Boudrieau, RJ. Fractures of the mandible. In: Johnson AL, Houlton JEF, Vannini R, eds. AO principles of fracture management in the dog and cat. Thieme, NY: AO Publishing, 2005. Boudrieau, RJ. Fractures of the maxilla. In: Johnson AL, Houlton JEF, Vannini R, eds. AO principles of fracture management in the dog and cat. Thieme, NY: AO Publishing, 2005. Nicholson, I, Wyatt, J, Radke, H, Langley-Hobbs, SJ. Treatment of caudal mandibular fracture and temporomandibular joint fracture-luxation using a bi-gnathic encircling and retaining device. Vet Comp Orthop Traumatol. 2010;23:102–108. Owen, MR, Langley Hobbs, SJ, Moores, AP, et al. Mandibular fracture repair in dogs and cats using epoxy resin and acrylic external skeletal fixation. Vet Comp Orthop Traumatol. 2004;17:189. Radiographs of the scapula should include lateral and caudocranial views. Lateral views may be obtained by placing the scapula dorsal to the vertebral column (preferred) or by superimposing the scapula over the cranial thorax. To avoid superimposing scapulae, the contralateral forelimb should be retracted away from the affected limb during the lateral projection. A distal-proximal or axial projection provides a skyline view of the scapular spine and cranial and caudal scapular borders. Because of the manipulation necessary for diagnostic radiographs, some animals may require sedation (see Tables 32-2 and 32-3 on pp. 1037-1038). Conservative treatment with a Velpeau sling (see p. 1052) and limited exercise are appropriate for most closed, minimally displaced fractures of the scapular body and spine in dogs that will heal rapidly. However, fractures of the articular surface must be treated with open reduction, anatomic alignment, and rigid fixation (see later discussion). Velpeau slings should be left on for no longer than 2 to 3 weeks, with care taken to prevent contracture of the carpus. Surgical treatment is indicated for unstable extra-articular fractures and for intra-articular fractures. Fixation systems applicable for scapular fractures consist of plates and screws, orthopedic wire, and Kirschner wires. The most appropriate fixation method should be determined on the basis of the fracture assessment score and fracture location; however, bone plates and screws offer the most stable fixation (Boxes 33-2 and 33-3). The overall health of the animal should be determined before surgery. Thoracic radiography and electrocardiographic analysis are warranted before anesthetic induction. Analgesics should be provided to posttraumatic animals (see Chapter 12). Refer to Tables 32-5 and 32-6 on pp. 1045-1048 for anesthetic management of patients with fractures. Palpable landmarks of the scapula are the spine, the acromial process, and the cranial, dorsal, and caudal borders. The body and spine of the scapula are easily approached with dissection and elevation of muscle. The neck of the scapula is surrounded by muscles and tendons that support the scapulohumeral joint (Fig. 33-16). Osteotomy of the acromial process allows reflection of a portion of the deltoideus muscle and visualization of the joint. The suprascapular nerve and artery course over the scapular notch and under the acromial process, and care should be taken to avoid these structures (see Fig. 33-16). The axillary artery and nerve are located immediately caudal to the joint but usually are not visualized with routine approaches. Approaches to the scapulohumeral joint are described on pp. 1257-1258. Excision arthroplasty and shoulder arthrodesis are discussed on p. 1258. Make a lateral skin incision extending the length of the spine distally to the shoulder joint (Fig. 33-17, A). Transect the omotransversarius muscle from the spine, and reflect it cranially. Incise the trapezius and the scapular parts of the deltoideus muscles from the spine and reflect them caudally. Incise the supraspinatus and infraspinatus muscular attachments to the spine, and elevate these muscles from the scapular body (Fig. 33-17, B).
Management of Specific Fractures
General Considerations and Clinically Relevant Pathophysiology
Diagnosis
Diagnostic Imaging
Medical Management
Interdental Stabilization Techniques
Application of Interdental Fixation
Application of Maxillomandibular Fixation
Surgical Treatment
Application of Interdental Wires
Application of Interfragmentary Wires
![]() TABLE 33-1
TABLE 33-1
GAUGE
MILLIMETER
INCH
16
1.25
.049
18
1.00
.040
20
0.80
.035
.032
.030
22
0.60
.028
24
.020
Application of Bone Plates and Screws
Application of External Skeletal Fixators
Acrylic fixators
Preoperative Management
Anesthesia
Surgical Anatomy
Surgical Technique
Open Reduction of Fractures of the Vertical Ramus and Temporomandibular Joint
Open Reduction of Maxillary Fractures
Stabilization of Mandibular Symphyseal Fractures
Stabilization of Mandibular Transverse Fractures
Stabilization of Oblique Fracture Lines
Stabilization of Comminuted Fractures
Postoperative Care and Assessment
Complications
Scapular Fractures
Diagnosis
Diagnostic Imaging
Medical Management
Surgical Treatment
Preoperative Management
Anesthesia
Surgical Anatomy
Surgical Technique
Approach to the Scapular Spine and Body
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Management of Specific Fractures