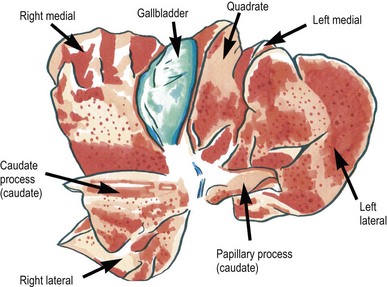
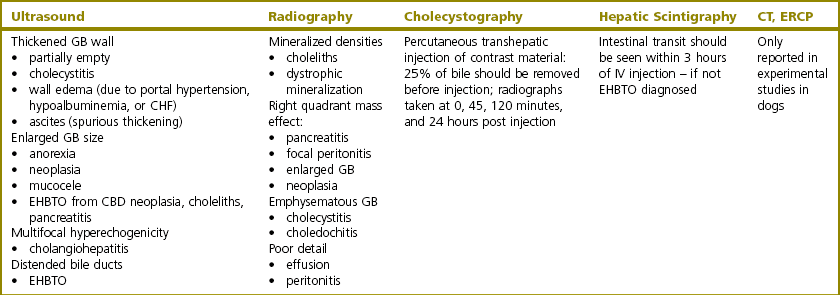
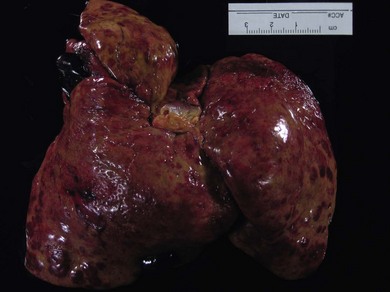
Chapter 31 While hepatobiliary disease is quite common in feline patients, diseases requiring surgery are relatively limited. Metabolic functions of the liver include production and excretion of bile, detoxification of numerous substances, as well as synthesis of plasma proteins.1 Diagnostic biopsy is most commonly performed as an isolated procedure or in conjunction with an abdominal exploration. Liver lobectomy (partial or complete) and diseases requiring biliary decompression, diversion, or cholecystectomy will be detailed. Anesthetic considerations and common complications following hepatic and biliary surgical procedures will be discussed. The feline liver consists of six lobes (Fig. 31-1). The liver may be further described by its visceral and parietal surfaces. The parietal surface is convex and abuts the diaphragm (Fig. 31-2) and the visceral surface is slightly concave and contacts the stomach, duodenum, and right kidney (Fig. 31-1). The gallbladder sits in the fossa between the right medial and quadrate lobes of the liver. The feline liver extends from the diaphragm into the xiphoid region between the left and right costal arches.2 The afferent blood supply of the liver consists of the high pressure arterial system as well as the low pressure portal system. The portal system supplies 80% of the blood to the liver while the remaining 20% of the blood is supplied by branches of the proper hepatic arteries.3 Efferent hepatic drainage is via the hepatic veins. Supporting ligaments of the liver include the right and left triangular ligaments (attaching to the muscular portion of the diaphragm), the right and left coronary ligaments (attaching to the central tendinous portion of the diaphragm), and the falciform ligament.4 Nervous supply to the liver is from afferent and efferent fibers of the vagus nerve and by sympathetic fibers of the celiac plexus.5 The biliary system consists of a gallbladder, cystic duct, common bile duct (CBD), hepatic ducts, segmental, septal, and interlobular bile ducts, bile ductules, and hepatic canaliculi.6 The gallbladder is made up of the larger fundus toward the apex and the infundibulum, or neck, which empties into the cystic duct.7 The gallbladder has four main functions: reservoir, absorptive, secretory and motor. Congenital biliary anomalies are seen commonly in cats (12.3%) and include partially divided gallbladders (bilobed, trilobed, or quadrupally divided gallbladder), double gallbladder, and a singular gallbladder with two or more ductular bladders.8 Most of these cases are found incidentally at necropsy. The cystic duct extends from the neck of the gallbladder to the junction with the first hepatic duct and continues distally as the CBD. The CBD continues to the duodenum, receiving more hepatic ducts along the way. In the dog, the CBD opens near the smaller of the two pancreatic ducts (the pancreatic duct). The larger duct is the accessory duct, which opens into the duodenum a few centimeters aborad on the minor duodenal papilla. In the cat, the CBD and the major pancreatic duct (which is the larger duct in this species) are usually fused prior to the entrance at the major duodenal papilla.1 The major duodenal papilla is approximately 3–6 cm aborad from the pylorus or 2 cm aborad from the junction of the CBD and the duodenal serosa. Some cats have varied anatomy, with the major pancreatic duct opening separately but immediately adjacent to the CBD. Approximately 2 cm caudal to the major duodenal papilla, the accessory pancreatic duct enters the duodenum at the minor duodenal papilla. This duct is sometimes absent in the cat. Pancreatic and biliary disease are commonly seen together in the cat because of this highly integrated anatomy.6,9 The circulation to the gallbladder and CBD is derived from the left branch of the proper hepatic artery.5 This circulation must be preserved during surgical procedures of the gallbladder in order to avoid necrotizing cholecystitis. The parasympathetic innervation of the gallbladder via the vagus nerve aids in contraction of the gallbladder and relaxation of the duodenal sphincter. The sympathetic innervation via the splanchnic nerves has the opposite effects.10 Filling of the gallbladder occurs continuously and bile flow is driven by hepatic secretion and gallbladder contraction. This is a low-flow, low pressure system. The sphincter of Oddi is the functional sphincter located at the terminal portion of the CBD. This sphincter demonstrates both tonic and rhythmic contractions and acts as a one-way valve to regulate pressure within the biliary system. It also provides resistance against retrograde passage of duodenal contents into the biliary tree. Spontaneous contraction of the gallbladder is also known to occur, which explains why serum bile acid values may appear higher after a 12 hour fast than during a two hour postprandial period.6 Diagnostics are usually initiated due to the presence of icterus or hyperbilirubinemia or clinical signs associated with hepatobiliary disease. Patients with extrahepatic biliary tract obstruction (EHBTO) are usually overtly icteric, have lost weight, and show symptoms of vague illness (anorexia, lethargy, etc.). Patients with clinical signs associated with necrotizing cholecystitis or septic bile peritonitis may present in shock, with diffuse abdominal pain or distension, icterus, and fever. Icterus is present when serum total bilirubin is greater than 2 mg/dL.7 Serum biochemical profiles can indicate cholestasis by increased serum transaminases (alanine aminotransferase, ALT; aspartate aminotransferase, AST), alkaline phosphatase (ALP), and gamma-glutamyl transpeptidase (GGT), and increased total bilirubin. ALP lacks steroid induction in cats, therefore any increase in ALP is referable to cholecystic disease but does not distinguish extrahepatic and intrahepatic causes. Hypercholesterolemia and bilirubinuria may also be seen with EHBTO patients.6,11 Radiography can be of use in selected cases of hepatobiliary disease.11 Liver size and configuration may be evaluated and hepatic masses can cause displacement of adjacent organs.12 Mineralized densities within the gallbladder, or choleliths, can be seen in approximately 50% of cases. Identification of radiopaque choleliths is not diagnostic for biliary obstruction as these may be an incidental finding in some normal animals.11 Dystrophic mineralization of the biliary tree can be seen in some cases of chronic cholangiohepatitis. Rarely, a mass or space-occupying lesion (pancreatitis, neoplasia, enlarged gallbladder) may be visible in the region of the CBD in cases of EHBTO. Diffuse peritoneal effusion seen on abdominal radiographs should encourage further diagnostics such as abdominocentesis to rule out bile peritonitis. Lastly, any presence of gas within the biliary structures or hepatic parenchyma indicates the presence of emphysematous cholecystitis or abscess, which should be surgically explored promptly. Cholecystography is not commonly performed in small animals, but experimental studies with different contrast agents have been conducted in the past. This procedure can be performed using iodinated contrast agents given orally (ipodate sodium/calcium, 150–500 mg/kg) or intravenously (5.2% iodipaminde meglumine, 0.3–1.0 mL/kg over 30 minutes); however, many variables affect the usefulness of this test and there is a potential for adverse reactions such as anaphylaxis and vomiting.6,11 Cholecystography is best used for diagnosis of choleliths, polyps, or biliary sludge. Percutaneous transhepatic cholangiocystography (PTC) also allows for direct visualization of the gallbladder and biliary tract but requires ultrasound guidance. Approximately 25% of the bile should be withdrawn prior to injection of contrast media and radiographs should be taken immediately, 45 minutes, 120 minutes, and 24 hours after injection.11 Abdominal ultrasound is an excellent tool for assessing the structures of the biliary tree and hepatic parenchyma. Contrast-enhanced ultrasonography has been used to help differentiate between benign and malignant hepatic nodules in a series of canine patients.13 Visualization of the normal gallbladder in cats can be difficult because the liver is oriented in a dorsoventral axis and displaced cranially under the ribs.11 Distension of biliary ducts and increased wall thickness of the gallbladder can be seen easily as the anechoic oval shape of the gallbladder is well recognized. A healthy gallbladder wall is usually poorly visible, as are biliary and hepatic ducts when not distended by disease. The CBD lies ventral to the portal vein and has a diameter of less than 4 mm in healthy cats.11 When thickening of the gallbladder wall is seen, many possibilities must be considered (Table 31-1). In one study an ultrasound measurement of the wall ≥1 mm was accurate in predicting gallbladder disease in cats.14 Enlargement of the CBD can occur within 24–48 hours of acute bile duct obstruction, whereas intrahepatic biliary duct distension requires five to seven days of obstruction. Cholelithiasis can be diagnosed by ultrasonography because both radiodense and radiopaque stones can be imaged but stones within the cystic or CBD can be difficult to visualize as they are not surrounded by anechoic bile and there is the presence of interference by intestinal or gastric gas. When studying a cohort of cats with spontaneous EHBTO, ultrasound detected a CBD > 5 mm in 97% of cats but only 50% of cats had a dilated gallbladder.15 Polyps, neoplastic masses such as adenomas or adenocarcinomas, or cysts within the gallbladder, cystic or CBD can be imaged via ultrasound although cystic hyperplasia with diffuse irregular wall thickening is more common. Due to the close anatomic association between the biliary and pancreatic systems, the pancreas should always be imaged when using ultrasonography. Pancreatic enlargement, focal steatitis or masses can cause EHBTO and treatment depends upon an appropriate preoperative diagnosis. For cats with suspected cholangitis or cholangiohepatitis, ultrasonography also allows for diagnostic testing to be performed, such as cholecystocentesis if the biliary tree is not pathologically affected. Percutaneous ultrasound-guided cholecystocentesis can be performed in cats and in one experimental study performed in healthy cats the risks of this procedure appeared to be low.16 Culture samples of bile yielded a significantly higher percentage of positive results when compared to hepatic cultures.17 Cholecystocentesis of a diseased or distended gallbladder increases the risks of complications, therefore biochemical analysis of blood, including a coagulation panel, should be considered before performing this procedure. All patients should be monitored for any signs of peritonitis for 24 hours after the procedure.18 In humans, severe vagal complications have been seen with diagnostic procedures of the gallbladder but this has not been reported in cats undergoing simple aspiration. Hepatic scintigraphy has been reported in small animals and involves the use of radioisotopes such as technetium (99mTc) attached to organic anions (iminodiacetic analogs). In humans, this modality can diagnose CBD occlusion, acute and chronic cholecystitis, segmental biliary tree obstruction, and sphincter of Oddi dysfunction.6 One study showed 83% sensitivity and 94% specificity for a diagnosis of biliary obstruction if no scintigraphic material was seen within the intestinal tract after passage of sufficient time for bile emptying (within three hours).19 Another study reported scintigraphic criteria for partial biliary obstruction in small animals.20 Disadvantages to this technique include limited availability, restrictions on patient handling, and the resultant delays to surgical intervention. Future diagnostic imaging modalities for use in cats may include computed tomography (CT), magnetic resonance imaging (MRI), as well as endoscopic retrograde cholangio-pancreatography (ERCP). CT and MRI may be used to delineate the extent of hepatic masses and show promise in distinguishing between benign and malignant processes.21 Three-dimensional spiral CT has been used in human studies of patients with suspected obstructive biliary disease.22,23 These studies have shown excellent results in diagnosing EHBTO compared to other current techniques such as PTC but have not been reported in our small animal patients to date. ERCP has only been reported in dogs to date. This combination modality uses endoscopy and fluoroscopy to identify the CBD and major pancreatic duct.24,25 This technique requires considerable training but is used commonly in humans to highlight masses, papillary stenosis, and choledocholiths. Thorough preoperative evaluation of patients undergoing hepatic or biliary surgery should include a complete blood count, biochemistry profile, urinalysis, and coagulation profile. Even though the liver has great regenerative capacity, the condition of the remaining liver determines how well removal of a portion of the liver may be tolerated. Diseases such as cirrhosis, prolonged biliary obstruction and hypoalbuminemia may result in reduced tolerance for removal of large amounts of liver tissue.7,26 Patients may be anemic and preoperative blood typing and access to blood for transfusion (see Chapter 5) as needed during surgery is warranted. Hypoglycemia as well as hypoalbuminemia may be encountered in patients with hepatic insufficiency.3 Animals with evidence of hepatic encephalopathy should be stabilized before proceeding with surgery. Decreased hepatic metabolism of drugs used to anesthetize patients should be taken into consideration (see Chapter 2). Doses of most drugs should be reduced and inhalant anesthetics are the preferred method of anesthestic maintenance.3 Use of propofol for anesthesia in cats with primary hepatic lipidosis did not appear to increase morbidity or mortality in a study of feline patients undergoing feeding tube placement.27 Prophylactic antibiotic usage is recommended for hepatic and biliary disease. Normally, the liver filters portal blood and bacteria may proliferate with hepatic ischemia or hypoxia.3,7 Cats with prolonged obstructive biliary disease are at risk for coagulopathies due to vitamin K malabsorption, which leads to deficiencies in factors II, VII, IX, and X.3,7 Any evidence of clinical bleeding or increases in prothrombin or activated partial thromboplastin times should receive vitamin K1 (0.1–0.2 mg/kg SQ once daily) for 24 to 48 hours before surgery or a plasma transfusion.3 Partial or complete biliary obstructions may allow ascending aerobic and anaerobic infection and subsequent bacteremia. The organisms most commonly isolated from biliary infections include Escherichia coli, Klebsiella spp., Enterobacter spp., Proteus spp., and Pseudomonas spp.3,7 Antibiotics that are excreted in an active form in the bile are most effective for treatment (see Box 31-1).3 Nutritional deficits should be considered (see Chapter 6), and placement of a feeding tube (see Chapter 12) either at surgery or preoperatively may be extremely important to aid in management of these cases.28 Anesthetic considerations (see Chapter 2) have been studied at length in animal models with regards to biliary surgery.29,30 Most importantly, systemic hypotension has been repeatedly discovered as a complication with obstructive jaundice.31,32 Loss of vascular responsiveness to sympathomimetic pressor agents with chronic bile duct obstruction is associated with systemic vasodilation and appears multifactorial.33,34 This lack of responsiveness to pressor support may make intraoperative and postoperative management of these patients challenging and in many studies postoperative hypotension has been linked to a poor prognosis.35,36 The association between obstructive jaundice and renal failure has also been well established in the human population and is associated with a mortality rate of 70–80% in people who develop it.37 Theories behind the cause of renal failure in this patient group include cardiovascular dysfunction (hypotension) leading to poor blood flow to the kidneys and acute renal tubular necrosis as a direct nephrotoxic effect of bile constituents. This functional hypovolemia may leave the kidneys more open to damage from endotoxemia and subsequent renal vasoconstriction as well.33 Traumatic injury to the hepatic parenchyma may lead to hemorrhage. Isolated hepatic injury is uncommon and small lacerations or fractures of the parenchyma rarely require surgical intervention, but severe trauma leading to hemorrhage that cannot be controlled with conservative or medical management may require exploratory surgery.7 Blunt trauma from automobiles is the most frequent cause of hepatic injury, although other rare causes such as hepatic rupture due to amyloidosis in six cats have been reported.38 A surgical technique that may be used to control hemorrhage includes temporary occlusion of the hepatic artery and portal vein through the epiploic foramen via the Pringle maneuver to slow hemorrhage by using either a finger or an instrument to compress the vessels.7 Other documented methods to control traumatic hemorrhage documented in human patients include direct suturing of intrahepatic vessels, resectional debridement, lobar resection, as well as perihepatic packing and replaparotomy.39 Hepatic cysts are epithelium lined cystic cavities in cats and dogs that have been associated with liver tumors, polycystic kidney disease, liver hydatidosis and congenital hepatopathies.40 Patients may be asymptomatic for cysts, present with abdominal pain, or a rare complication, seen in humans, may be biliary obstruction.41 In a study reporting on nine cats with hepatic cysts, the common presenting clinical signs were anorexia, reduced activity, and vomiting. All patients had abdominal pain on palpation. Four out of nine cats had concurrent renal cysts. Ultrasound-guided drainage and alcoholization of the hepatic cysts was reported, with a low rate of complication and amelioration of clinical signs.40 Other reported treatments include partial lobectomy, excision of the cystic membrane, as well as omentalization.42,43 Hepatic cysts have also been reported in conjunction with peritoneopericardial diaphragmatic hernia in a cat.44 Hepatic abscesses may form as isolated lesions, manifestations of systemic infections, or as diffuse microabscesses.45 In human patients most abscesses are bacterial in nature and most commonly affect the right liver lobes. This may be due to its proximity to the biliary tree or the portal anatomy that permits translocation of intestinal flora.46–48 In a study of 14 cats with reported hepatic abscesses, the overall mortality rate was high at 79%. Polymicrobial growth was cultured from 66% of the cats, with E. coli most frequently isolated.45 Feline patients often present with non-specific clinical signs such as anorexia, lethargy and weight loss. Most affected cats were septic and many were hypothermic. In dogs with hepatic abscessation, 100% of patients were reported to have had an increase in serum ALP activity, while this study reported 50% of feline patients failed to have an increase in serum liver enzymes.49 Most of the feline cases reported had multiple macroscopic abscesses, but the survival rate was higher (75%) in the cases where a solitary abscess was found which was surgically resected. Results were favorable in one cat treated with percutaneous ultrasound-assisted drainage and alcoholization of a focal hepatic abscess.50 Hepatic lobe torsion is exceptionally rare and has only been reported in one cat.4 The left side of the liver is most commonly affected in dogs, with one study documenting a left lateral lobe torsion in 48% of animals4 and the left medial lobe was most commonly affected in another study of 13 dogs.51 The supposition is that the left lateral lobe is the largest, most well defined and most mobile of all hepatic lobes.52,53 While an underlying cause for liver lobe torsion is often never found, one feline case report documented torsion of the right medial liver lobe, and the lobe contained a ruptured hepatocellular carcinoma.4 This patient was presented to an emergency hospital in respiratory distress with dyspnea as well as anemia and hemoperitoneum. The patient was euthanized due to poor condition and the torsion was documented on postmortem examination. This is in contrast to dogs, where a good long-term outcome for dogs undergoing surgery for liver lobe torsion has been reported.51 Other reported causes may include congenital absence or traumatic rupture of the supporting ligaments of the liver.54,55 Liver neoplasia may be primary or due to metastatic disease. Tumors may arise from hepatocytes, bile duct epithelium, neuroendocrine cells or stromal cells.56 Tumors generally occur in older animals and presenting clinical signs are generally non-specific.58 Cats with malignant tumors, though, are more likely to show clinical signs of illness than those with benign masses, and overall benign masses seem to be more common than malignant tumors.58 In a study of 41 cases of cats with primary hepatobiliary masses, the most common malignant tumor type was found to be cholangiocellular carcinoma and the most common benign masses were cholangiocellular adenomas, hepatocellular adenomas, and biliary cysts (Fig. 31-3).58 Cats with benign disease that underwent exploratory surgery had no complications or recurrence documented at two months following surgery, yet 86% of cats with malignant disease were euthanized or died during surgery.58 Benign hepatic nodular myelolipomatosis has been reported in conjunction with a peritoneopericardial diaphragmatic hernia.59 Reported survival following surgical excision of a solitary myelolipoma was favorable.60 Carcinomas of the biliary system in cats behave aggressively and one report documented an 80% rate of metastasis.61 Hepatobilliary neuroendocrine carcinoma has been studied in 17 cats, and was associated with a poor prognosis, with 14/17 cats being euthanized during or immediately after surgery.57 Treatment for solitary tumors is partial or complete liver lobectomy (see liver lobectomy information section below). Local lymph nodes should be evaluated for metastatic disease. In patients where diffuse neoplastic disease is present, liver biopsy is warranted (see liver biopsy information section below) (Fig. 31-4). In two reports, the liver was involved in 20–24% of cats with lymphocytic lymphoma (Fig. 31-5).62,63 Radiographic and ultrasound imaging can document the location and extent of hepatic tumors.64 Additional imaging such as CT and MRI may be useful to determine resectability of a tumor and three-view thoracic radiographs should be taken to look for pulmonary metastatic disease.56 Non-resectable and metastatic liver disease may be treated with novel techniques such as regional chemoembolization.65 Liver biopsy is commonly performed as a solitary procedure or in conjunction with an abdominal exploratory procedure (see Chapter 23). There are many indications for hepatic biopsy, including liver enzyme elevation for more than 30 days, ultrasonographic lesions, disease staging, and previous non-diagnostic cytologic study.66 For diffuse hepatic disease, such as lipidosis (Fig. 31-6) or neoplasia, cytology may provide an adequate diagnosis, but fails to show architectural details that can only be obtained via histopathology. One study documented agreement between cytologic and histopathologic diagnosis of liver disease in only 51% of feline patients.67 Another study documented several cats incorrectly diagnosed with only hepatic lipidosis instead of lymphosarcoma.68 As cytology provides only a small sample size and does not detail parenchymal architecture, hepatic biopsy is generally favored. Multiple techniques exist and each method has advantages and disadvantages. Less invasive methods are ideal but may provide only small tissue samples, yet general anesthesia may be needed to obtain larger specimens. Techniques reported for obtaining a liver biopsy including loop guillotine suture (Fig. 31-7), punch biopsy, ultrasonically activated scalpel (which can be used in both open and laparoscopic fashion), as well as stapling methods.3,7,69 The loop suture method is adequate for sampling the margin of the liver, while a skin punch biopsy is ideal for focal lesions within the central portions of the liver. Absorbable gelatin foam (Gelfoam Pfizer, New York), a mattress suture, or omental tissue may be used to control hemorrhage.7 Use of tissue forceps is avoided in grasping the specimen to avoid creating a crushing artifact. Surgically obtained wedge samples should be at least 1 cm, preferably 2 cm deep, as subcapsular tissue contains more fibrous tissue and can be misleadingly interpreted as representing the entire liver.70 An ideal liver biopsy should be of adequate size and taken from a location that is representative of the primary liver pathology. At least two to three samples should be obtained from separate liver lobes, including both peripheral and central locations, as well as grossly normal and abnormal-appearing tissue.70 Human studies suggest that at least six to eight portal triads must be obtained for adequate histopathologic interpretation.71 Ultrasound-guided needle-core biopsy techniques are minimally invasive, but they require a skilled ultrasonographer, do not allow access to all areas of the peritoneal cavity, and have been shown to produce inferior samples in many cases when compared with open surgical or laparoscopic techniques.72 In a study of 124 animals, the morphologic diagnosis assigned to needle biopsy specimens agreed with that of the wedge biopsy only 48% of the time.73 Additionally, a high rate of complications using an automatic Tru-Cut biopsy device in 26 cats has been reported. In that study, 19% of the cats developed fatality following biopsy, attributed to a pressure wave that may have caused a vagal mediated shock.74 Laparoscopic biopsy (see Chapter 24) is an ideal method for acquiring a larger sample size (Fig. 31-8). This technique allows for magnified visualization of hepatic pathology as well as permitting observation of the sites following biopsy to be monitored for hemorrhage (Fig. 31-9). In addition, laparoscopy has proven safe and effective for providing accurate specimens of hepatic parenchyma.69,75 While laparoscopy is performed under general anesthesia, the time of the procedure is rapid, with a mean reported surgery time of 35 minutes.75 Samples from laparoscopic biopsy forceps are usually about 5 mm in diameter, depending on surgeon technique and depth of penetration. Laparoscopic cup biopsies provide about 45 mg of tissue, a 14G Tru-Cut-type biopsy needle provides 15–20 mg, and an 18G needle biopsy provides only 3–5 mg of liver tissue.70 Disadvantages of the laparoscopic biopsy include the expense of equipment and the expertise needed, but the advantages over open laparotomy are significant, including faster patient recovery, lower postoperative morbidity, decreased infection rate, less postoperative pain, and decreased hospitalization time.70,72
Liver and biliary tract
Surgical anatomy
Biliary anatomy and flow
General considerations
Diagnostic tests
Diagnostic imaging
Presurgical considerations
Surgical diseases of the liver
Hepatic trauma
Hepatic cysts
Hepatic abscess
Liver lobe torsion
Hepatobiliary neoplasia
Surgical procedures of the liver
Liver biopsy
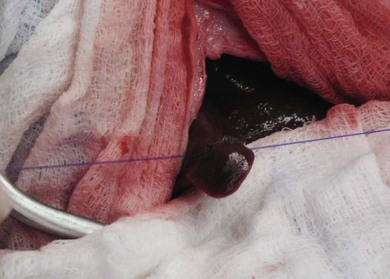
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Liver and biliary tract