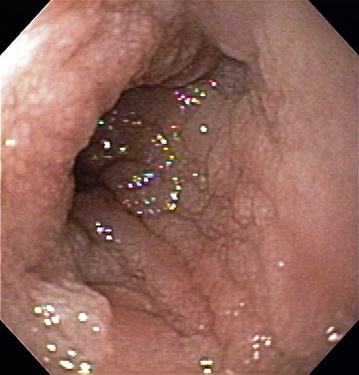
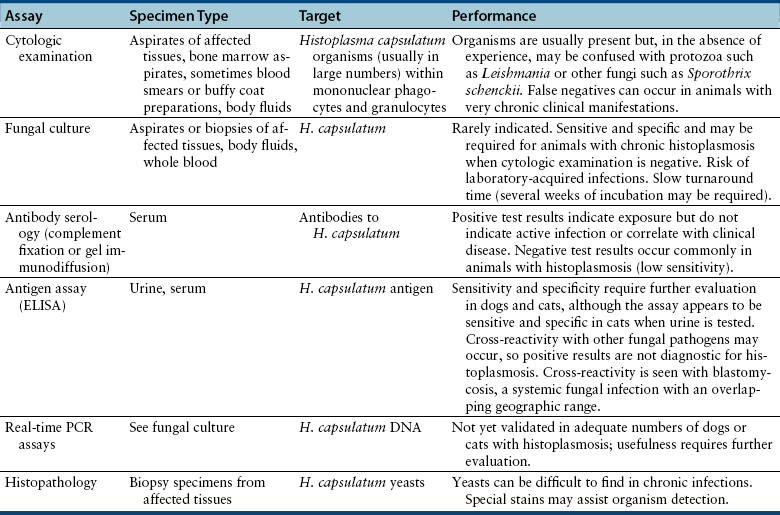
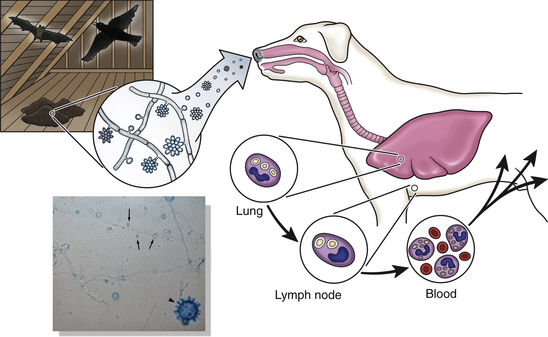
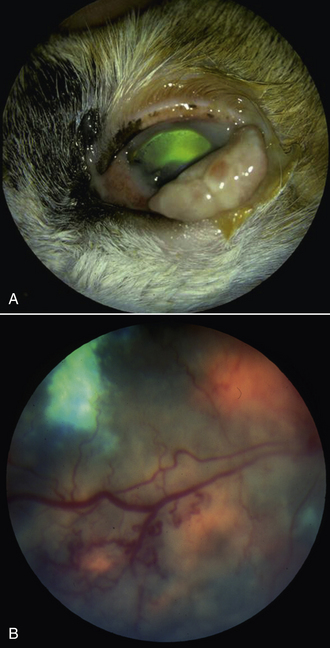
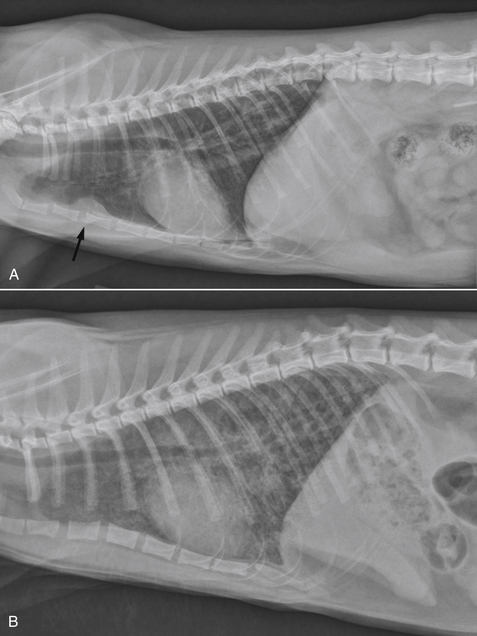
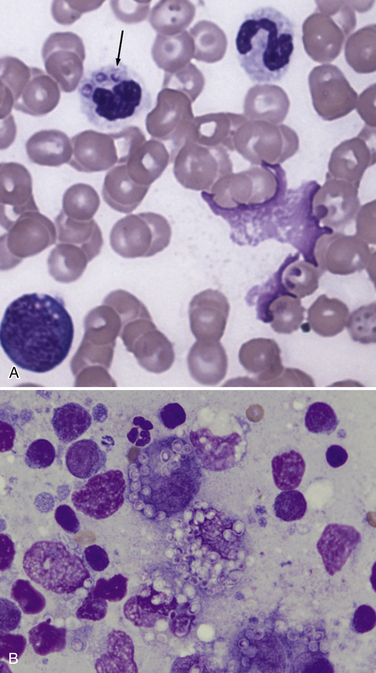
Chapter 61 Histoplasma capsulatum is a dimorphic, soil-borne fungus that is found worldwide, but especially along the Mississippi, Missouri, Tennessee, and Ohio river valleys of the United States, as well as in Latin America (Figure 61-1). Endemic areas within the United States span the central portion of the United States from western Virginia to central Texas. Disease has also been reported in cats or dogs from northern California2; Brazil3; Italy4; Queensland in Australia5; Japan6; and western Canada.7,8 Eight clades of the organism have been identified by genetic analysis: North American (class 1 and class 2), Latin American (group A and group B), and one each of Australian, Indonesian, Eurasian, and African. These may vary in virulence. All except the Eurasian clade, which is derived from the Latin American group A clade, may be distinct phylogenetic species.9 A possible ninth clade, which is related to, but distinct from, North American class 1 also appears to infect cats in North America outside the accepted endemic range.10 Three variants have also been described based on pathogenicity and morphology—H. capsulatum var. capsulatum, H. capsulatum var. duboisii, and H. capsulatum var. farciminosum—although the phylogenetic value of these variants has been debated.6,9 H. capsulatum var. duboisii occurs primarily in Africa and Japan. H. capsulatum var. farciminosum infections occur primarily in horses, but have also been reported in humans and dogs. H. capsulatum grows best in soil where temperatures are between 22°C and 29°C, where annual rainfall is 35 to 50 inches, and where relative humidity is 67% to 87%. These conditions are typically found between latitudes of 45 degrees north to 30 degrees south.11 H. capsulatum can be found in the intestinal tracts and guano of bats, which are the primary reservoir of the organism and serve to disseminate it geographically.12 Bat caves can maintain perfect growth conditions for H. capsulatum. Although H. capsulatum can be found in high concentrations in decaying avian guano (especially around blackbird or starling roosts and chicken coops), it is not found in fresh feces or shed in the feces of birds. Cats are as susceptible, or slightly more susceptible, to histoplasmosis than dogs. Affected cats can be as young as 2 months and, in some cases, older than 15 years.13 The mean age of affected cats has varied from around 4 years to 9 years.14 For dogs, a mean age of 4.3 years was reported (range, 5 months to 10 years).15 Dogs in the 2- to 4-year and 4- to 7-year age groups were more likely to develop histoplasmosis than dogs less than 2 years of age.16 Sporting or working dogs may be at greater risk of infection because of increased exposure; in a study using the Veterinary Medical Database, pointers were strongly overrepresented.16 Weimaraners and Brittany spaniels were also at increased risk. Among cats, Persian cats may be slightly overrepresented. A sex predisposition has not been clearly identified in dogs or cats, but more female than male dogs were affected in some case series.14,15,17–19 This contrasts to human histoplasmosis and other systemic mycoses in dogs, which affect males more often than females.20 The overwhelming majority of cats with histoplasmosis are retrovirus negative, but a significant percentage of cats in two studies (16% and 28%, respectively) were co-infected with FeLV.13,14 A small percentage of cats have underlying comorbidities such as lymphoma, feline infectious peritonitis, or a history of glucocorticoid treatment.13 Comorbidities described in dogs include dirofilariasis15 and metastatic carcinoma.6 Disease can occur in cats that are housed exclusively indoors. In the soil, the mycelial phase of H. capsulatum forms macroconidia and microconidia (Figure 61-2). The microconidia are thought to be the form inhaled by mammalian hosts, because they are small enough (2 to 5 µm) to enter the terminal bronchioles and alveoli. Within the lungs (i.e., at a temperature of 37°C), the microconidia transition to a unicellular yeast, which replicates by budding. The fungus binds to CD11-CD18 integrins on alveolar macrophages and is phagocytized. It then replicates within these cells through control of the phagolysosomal environment and ultimately destroys them, with subsequent replication in other resident alveolar macrophages and inflammatory phagocytes that are recruited to the lung.21 Acquisition of iron by the fungus is essential for growth in vivo.22 Some animals control the initial infection but remain latently infected with small numbers of yeasts. Subsequent immune suppression can lead to reactivation of infection years later. Thus, the incubation period can range from 2 to 3 weeks to as long as several years. FIGURE 61-2 Life cycle of Histoplasma capsulatum. In the environment, the organism forms macroconidia (arrowhead, inset) and microconidia (arrows, inset). The microconidia are thought to be inhaled into the lungs of mammalian hosts. Within the lung, the organisms transform into yeasts that infect alveolar macrophages and then disseminate to local lymph nodes and the systemic circulation. The clinical manifestations and rate of disease progression depend on the host immune response to infection, the infectious dose, and the Histoplasma strain, which can vary geographically. The vast majority of infections are probably subclinical.23 Replication of the organism leads to a granulomatous inflammatory response in the lungs. Occasionally, the inflammatory response is followed by fibrosis and scarring. The yeasts migrate to local lymph nodes (such as the hilar lymph node) and other tissues that contain mononuclear cells, such as the liver and spleen. When the cell-mediated immune response is defective or absent, disseminated disease occurs (referred to in human patients as progressive disseminated histoplasmosis [PDH]20), which may be acute or chronic. In addition to lymph nodes, liver, and spleen, other common sites of dissemination are the bone marrow, small and/or large intestinal tract, pancreas, skin, bones, central nervous system (CNS), and eyes. Dogs with histoplasmosis in the United States appear to be particularly susceptible to intestinal involvement. Severe infiltration of the small and large intestines leads to malabsorption, diarrhea, severe weight loss, and hematochezia, often without evidence of respiratory involvement. Clinical signs in cats are commonly vague and nonspecific, such as weight loss, inappetence, weakness, dehydration, and fever.13,14 Approximately 40% of cats show respiratory signs such as dyspnea and tachypnea, and to a lesser extent, cough and nasal discharge. However, respiratory signs may be absent in some cats with dissemination of infection to nonpulmonary sites. Ocular signs such as chorioretinitis and/or posterior or anterior uveitis occur in approximately one quarter of cats with histoplasmosis, and around 20% of cats have signs of skeletal involvement.13,14,17 Nodular or ulcerated and draining skin lesions, peripheral lymphadenopathy, vomiting, diarrhea, oral ulceration, myelopathy, and/or hematuria due to bladder wall involvement have also been reported.4,14,17,24–29 Clinical signs associated with gastrointestinal involvement are much less likely to occur in cats than in dogs. A high proportion of affected cats that were necropsied had severe disseminated disease.13 In dogs, diarrhea, decreased appetite, weight loss, lethargy, fever (up to 40°C or 104°F), and mucosal pallor are the most common clinical signs.7,8,15,18 In addition to inappetence, weight loss, and diarrhea, other clinical signs referable to the gastrointestinal tract include melena, tenesmus, hematochezia, dyschezia, and/or increased frequency of defecation.8,15,18 Profuse diarrhea may be chronic and persist for several months. Hilar lymphadenopathy is common, and may be an incidental finding on thoracic radiographs, or it may be severe and contribute to signs of cough. Other signs include respiratory difficulty, icterus, vomiting, hepatomegaly, lymphadenomegaly, nasal discharge, ocular signs, polyuria and polydipsia, lameness due to osteomyelitis, and neurologic signs such as seizures or paralysis/paresis.8,15,30–32 Affected dogs in Japan have had chronic cutaneous or gingival lesions in the absence of pulmonary or gastrointestinal involvement,33–36 although disseminated disease has also been described.6 Skin nodules were also reported in an Australian dog with histoplasmosis.5 Varied clinical manifestations of histoplasmosis in different parts of the world as a result of strain variation in H. capsulatum also occur in humans.20 Physical examination findings in cats with histoplasmosis can be minimal or can include thin body condition or emaciation; fever; pale and/or rarely icteric mucous membranes; peripheral lymphadenopathy; respiratory signs such as dyspnea, tachypnea, and increased or decreased lung sounds; single or multiple cutaneous nodules, ulcerations, and/or draining tracts (Figure 61-3); lameness; and detection of organomegaly, abdominal masses, and/or pain on palpation of the abdomen. Ocular signs include chorioretinitis, optic neuritis, anterior uveitis, retinal detachment, panophthalmitis, and glaucoma (Figure 61-4). FIGURE 61-3 Cutaneous lesion on the eyelid of a cat with histoplasmosis. (Courtesy Dr. Amy Grooters, Louisiana State University.) FIGURE 61-4 Ocular changes in cats with histoplasmosis. A, Blepharitis. B, Granulomatous chorioretinitis with multifocal pigmented lesions. (A, From Ketring KL, Glaze MB. Atlas of Feline Ophthalmology. 2nd ed. Hoboken, NJ: Wiley-Blackwell; 2012. B, Courtesy of Dr. Mary Belle Glaze, Gulf Coast Animal Eye Clinic, Houston, TX.) In dogs, lethargy, fever, thin body condition, and pale mucous membranes are most often found on physical examination. Other physical examination abnormalities include dehydration, hepatomegaly, icterus, and/or ascites; tachypnea, increased respiratory effort, and increased lung sounds; lymphadenomegaly that involves one or more peripheral lymph nodes; abnormal stool quality on rectal examination (diarrhea, hematochezia, or melena); nasal and ocular discharge; tachycardia; tongue lesions; and cutaneous nodules, ulceration, or draining tracts.5,8,15,18,30,37,38 Ocular examination can reveal uveitis, evidence of optic neuritis, or chorioretinitis with retinal detachment.18,39,40 One dog was seen for lameness, hyperemia, and edema of the left pelvic limb because of a sclerosing pyogranulomatous inflammatory mass in the inguinal region that resulted in venous occlusion.37 Rarely, neurologic signs such as ataxia, obtundation, head tilt, nystagmus, strabismus, seizures, facial paralysis, and tetraparesis may be present on physical examination as a result of hepatic encephalopathy or meningoencephalitis.40–42 The CBC in dogs and cats with histoplasmosis reflects the presence of systemic inflammation, gastrointestinal hemorrhage, and/or bone marrow infiltration by fungal organisms. In both dogs and cats, anemia is a common abnormality, may be mild to severe, and is usually normocytic, normochromic, and nonregenerative.14,15,17,18,43,44 Increased numbers of nucleated erythrocytes occur in some affected dogs.8,44 The total white cell count or neutrophil count may be normal, increased, or decreased.15,17,18,43 Most affected cats have a normal or decreased white cell count,14,43 but leukocytosis due to neutrophilia and monocytosis may be more common in affected dogs.15,44 Increased numbers of band neutrophils with toxic neutrophils, lymphopenia, monocytopenia, and thrombocytopenia can be present in some severely affected animals.14,17,18,43,45 Thrombocytopenia can be a result of platelet consumption, sequestration, and/or myelophthisis. Rarely, eosinophilia is present.46 Mild to severe hypoalbuminemia is present in most (>75%) affected dogs and cats. Cats with liver involvement may have increased activities of serum ALT and AST.17,43 Hyperbilirubinemia and increased serum ALP activity are rarely reported.17 Hypercalcemia and hyperglobulinemia have been described in a few affected cats.17 Hyperglobulinemia; mild to moderate increases in the activity of serum ALT, AST, ALP, and GGT; and hyperbilirubinemia can be found in dogs. A few dogs with acute PDH have had coagulation abnormalities characterized by increased PT and PTT and fibrin degradation product or D-dimer concentrations.31,44 Coagulation abnormalities in dogs with histoplasmosis may result from disseminated intravascular coagulation and possibly severe hepatic involvement (see also Canine Case Example). In cats, thoracic radiographic findings in histoplasmosis usually consist of diffuse, linear, nodular, or miliary interstitial patterns, but mixed interstitial-alveolar-bronchial patterns, pleural effusion, or an absence of abnormal findings can also occur (Figure 61-5).14,19,43,47 Plain thoracic radiographs in dogs may show alveolar, interstitial, and/or bronchial patterns, tracheobronchial lymphadenopathy, lung lobe consolidation, and/or rarely pleural effusion.31,45,47,48 Lesions in dogs sometimes mineralize, which does not seem to occur in cats. Abdominal radiographs may show hepatomegaly, splenomegaly, or decreased serosal detail due to ascites. Radiographic evidence of osteomyelitis may be present in cats, with associated soft tissue swelling and sometimes pathologic fractures. Osteomyelitis is rarely described in dogs.30,32 FIGURE 61-5 Radiographic abnormalities in feline pulmonary histoplasmosis. A, Lateral thoracic radiograph from an 8-month-old intact male domestic shorthair cat with disseminated histoplasmosis. There is a diffuse bronchointerstitial pulmonary pattern and evidence of sternal lymphadenopathy (arrow). In the viewable abdomen, marked splenomegaly can be appreciated. B, Lateral thoracic radiograph from a 7-month-old male neutered domestic shorthair cat with histoplasmosis that was evaluated for tachypnea and dyspnea of 10 days duration. There is a diffuse, severe, interstitial-to-coalescing and patchy pulmonary pattern that obscures visualization of the pulmonary vasculature and cardiac contours. (Courtesy of Lorrie Gaschen, Louisiana State University.) Findings on abdominal sonographic examination of dogs with histoplasmosis include hepatic enlargement and hypoechogenicity, abdominal lymphadenopathy, splenomegaly, and ascites. A thickened intestinal wall may be present with disruption of bowel wall architecture. Adrenomegaly, abdominal lymphadenopathy, and occasionally renomegaly have been described in cats.14 Diagnostic assays currently available for histoplasmosis in dogs and cats are described in Table 61-1. Cytologic examination of aspirates or impression smears of affected tissues (e.g., fine-needle aspirates of liver, spleen, lymph nodes, lung, bone marrow), rectal scrapings, or Cytospin preparations of lung wash specimens or body fluids (e.g., CSF, synovial fluid, ascites, or pleural effusion) usually reveals pyogranulomatous or granulomatous inflammation. H. capsulatum yeasts can be seen extracellularly and intracellularly (usually within mononuclear phagocytes). Most extracellular organisms are probably an artifact of smear preparation. Occasionally one or more organisms are seen in circulating monocytes, neutrophils, or eosinophils in severely ill animals with disseminated disease (Figure 61-7). Cytologic evidence of fungemia was detected in nearly 20% of affected cats in one study.13 The bone marrow is a common site to yield organisms in cats, even when hematologic abnormalities are minimal. FIGURE 61-7 A, Blood smear from a dog with Histoplasma capsulatum fungemia. Three organisms can be seen in a circulating neutrophil (arrow). Wright’s stain, 1000× magnification. B, Fine-needle aspirate cytology from the right popliteal lymph node of the cat in Figure 61-5, A. There is pyogranulomatous inflammation with large numbers of intracellular yeast organisms with morphology consistent with that of H. capsulatum. Wright’s stain, 1000× magnification. (Courtesy Angela Royal, Louisiana State University.)
Histoplasmosis
Etiology and Epidemiology
Clinical Features
Physical Examination Findings

Diagnosis
Complete Blood Count
Serum Biochemical Tests
Coagulation Testing
Diagnostic Imaging
Sonographic Findings
Microbiologic Tests
Cytologic Examination
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Histoplasmosis
Only gold members can continue reading. Log In or Register to continue