Induction to Anesthesia (Dosages in Table 23.2)
Standard protocols like diazepam/ketamine, guaifenesin/ketamine, or tiletamine/zolazepam are all appropriate, and no changes in dose or technique are required for horses undergoing laparoscopy.
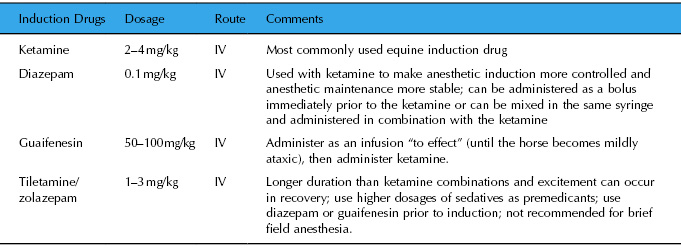
Table 23.2 Drugs used for anesthetic induction in equine anesthesia
Maintenance of Anesthesia
Once induced to anesthesia, the horse should be immediately intubated and the endotracheal tube cuff should be inflated. The horse should be placed on a padded table with its weight equally distributed across the dependent muscle groups. Laparascopic surgeries are generally of sufficient duration that inhalant anesthetics, rather than injectable anesthetics, should be used for maintenance of anesthesia. Both isoflurane and sevoflurane are appropriate inhalants for maintenance of anesthesia in the horse. The dosage of the inhalant anesthetic should be kept as low as possible since the inhalants produce dose-dependent adverse effects, like hypotension and hypoventilation, which can have a major negative impact on the patient. Injectable anesthetic drugs often cause less cardiovascular depression than inhalant drugs (McMurphy et al. 2002; Yamashita et al. 2007) and total injectable venous anesthesia (TIVA) may be appropriate for some procedures. However, inhalant drugs require minimal metabolism for the termination of their effects, whereas injectable drugs require moderate to extensive metabolism for termination of effects. In long procedures, the injectable drugs can accumulate in the horse and this will result in delayed recovery. Thus, TIVA is generally only appropriate for short procedures. Even if TIVA is chosen over inhalant anesthesia, the horse must be endotracheally intubated and placed on ventilatory support, as described below.
Anesthetic drugs, surgical positioning, and pneumoperitoneum following insufflation of the abdomen all have a major impact on the cardiovascular and respiratory systems; thus, monitoring and appropriate support of these systems should begin as soon as the patient is positioned on the surgical table. In anesthetized horses, accurate assessment of the cardiovascular and respiratory systems cannot occur without direct measurement of arterial blood pressure and assessment of arterial blood gases, and an indwelling catheter should be placed into an artery immediately after induction to anesthesia. Pulse oximeters and capnometers should also be used to monitor oxygen–hemoglobin (SpO2) saturation and end-tidal carbon dioxide (ETCO2), respectively. However, these monitors provide only trends, and not necessarily accurate numbers, in anesthetized horses (Koenig et al. 2003). Also, because of the shape of the oxygen–hemoglobin dissociation curve, the pulse oximeter should not be considered a monitor of ventilation but rather a monitor of oxygenation, meaning that patients can be well oxygenated—especially on 100% oxygen—but not necessarily ventilating normally. Additionally, horses commonly develop ventilation/perfusion (V/Q) mismatch under anesthesia, and this will adversely affect the accuracy of the ETCO2 monitor. Thus, assessment of arterial blood gases is required in anesthetized horses, especially those undergoing laparoscopy with insufflation. A standard lead II electrocardiogram should also be monitored as the hypoxemia and hypercarbia that commonly occur in dorsally recumbent horses with pneumoperitoneum can cause arrhythmias.
Most importantly, the maintenance phase of anesthesia should be kept as short as possible since the risk of anesthesia-related morbidity and mortality exponentially increases as the duration of the procedure increases (Richey et al. 1990; Johnston et al. 1995,1996; Bidwell et al. 2007).
Support of the Respiratory System
Most anesthetic drugs, especially the inhalant drugs, cause some degree of respiratory compromise. In addition, most horses anesthetized for laparoscopic surgery are placed in dorsal recumbency and horses in dorsal recumbency are more likely to be hypoxemic than horses in lateral recumbency (Steffey et al. 1977; Gasthuys et al. 1991; Day et al. 1995). This occurs because anesthetized, recumbent horses commonly develop V/Q mismatch, in which the dependent portions of the lung become atelectatic and are perfused but not well ventilated, while the nondependent portions of the lung are aerated and well ventilated but poorly perfused (Nyman & Hedenstierna 1989; Nyman et al. 1990). Horses placed in Trendelenberg position develop a greater degree of hypoxemia, hypercarbia, and V/Q mismatch whether or not pneumoperitoneum is induced (Duke et al. 2002). Horses with pneumoperitoneum during insufflation for laparoscopy have further respiratory compromise and become hypoxemic, hypercarbic, and acidotic (Donaldson et al. 1998). This is due in part to physical impingement on the caudal lung fields by the distended abdomen and in part due to absorption of a portion of the CO2 insufflation gas from the abdomen into the bloodstream (Henny & Hofland 2005).
To prevent or alleviate hypoxemia and hypercarbia, intermittent positive-pressure ventilation (IPPV) should be instituted as soon as possible following induction to anesthesia. IPPV is most effective when instituted prior to the onset of V/Q mismatching. IPPV initiated after the onset of hypoxemia may not improve arterial oxygen (PaO2) in dorsally recumbent horses (Day et al. 1995). Ventilator settings of 5–10 breaths/min with a tidal volume of 10 mL/kg, a peak inspiratory pressure of 20–30 cmH2O, and an inspired : expired (I : E) ratio of 1 : 3 will generally provide effective ventilation until the abdomen is fully insufflated. At that point, peak airway pressure may need to be increased to provide adequate inflation of the lung; however, this may have a significant impact on cardiovascular function (see following section). An alternative is to decrease the tidal volume and increase the respiratory rate during peak insufflation time. The PaO2 may decrease with this technique because the lower tidal volume and airway pressure will allow more alveoli to become atelectatic, but the technique will minimize the impact of IPPV on the cardiovascular function. Normal values for PaO2 and PaCO2 are listed in Table 23.3.
Table 23.3 Normal physiological values in anesthetized horses
| Variable | Normal Value | Comment |
| Mean arterial blood pressure | 70 mmHg | Mean arterial pressure below 70 mmHg has been associated with postoperative myopathy. |
| Arterial oxygen content (PaO2) | >200 mmHg | Ideal PaO2 is five times inspired oxygen content, which would be 500 mmHg on 100% oxygen. Hypoxemia is defined as PaO2 <60 mmHg. |
| Arterial carbon dioxide content (PaCO2) | 35–55 mmHg | Normal PaCO2 in the conscious horse is 35–45 mmHg, but some degree of respiratory depression is tolerated under anesthesia. PaCO2 >55–60 mmHg will contribute to respiratory acidosis and should be corrected with appropriate ventilatory support. |
Support of the Cardiovascular System
Almost all anesthetic drugs cause some degree of cardiovascular compromise and horses are at greater risk than other species for developing anesthesia-induced cardiovascular dysfunction (Wagner 2000). Furthermore, dorsal positioning, pneumoperitoneum, and IPPV all cause cardiovascular changes. Dorsal positioning causes a decrease in mean arterial blood pressure, cardiac output, and stroke volume (Gasthuys et al. 1991). Pneumoperitoneum during laparoscopic insufflation causes an increase in cardiac work, which could put patients with poor cardiovascular function at an increased risk for developing cardiovascular compromise (Donaldson et al. 1998). Finally, ventilatory support required to overcome respiratory complications in the anesthetized dorsally recumbent horse will further compromise cardiovascular function by causing a decrease in arterial blood pressure and cardiac output (Edner et al. 2005).
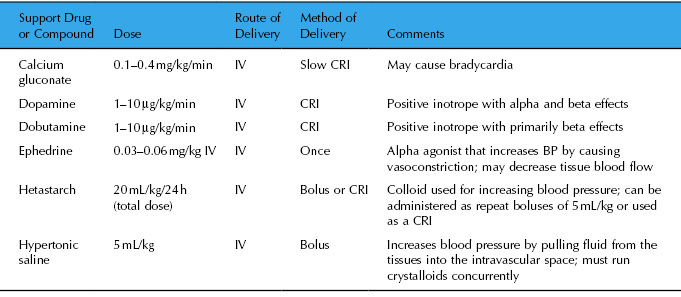
Hypotension (mean arterial blood pressure <70 mmHg; Table 23.3) has been identified as the primary risk factor for postanesthetic myopathy (Richey et al. 1990) and neuropathy, and blood pressure support should be initiated rapidly and aggressively if hypotension occurs. IV fluids are used to treat inhalant-induced hypotension as well as to replace fluid losses from surgery, urine production, and insensible losses through the airway and sweating. Balanced electrolyte crystalloids (e.g., lactated Ringer’s solution [LRS] or Normosol-R) are the fluids of choice, and an administration rate of 10 mL/kg/h is adequate for healthy patients anesthetized for routine procedures with minimal blood loss. The rate should be increased if the patient is dehydrated or hypovolemic, hypotensive, or hemorrhaging. Hypertonic (7.5%) saline can be administered if the hypotension is severe or unresponsive to other treatment options. However, because of the depression of myocardial contractility induced by inhalation anesthetics, IV fluids alone may not be sufficient to maintain acceptable cardiac output and blood pressure (Wagner 2000). In this instance, positive inotropic drugs, which increase myocardial contractility, should be utilized. Calcium, dopamine, dobutamine, and ephedrine are the most commonly used inotropes in the horse. Dosages for support drugs and comments regarding selection of specific inotropes are listed in Table 23.4.
Table 23.4 Support drugs and compounds used in anesthetized horses
Other Considerations
Horses placed in the Trendelenburg position rapidly develop edema in the head and in the upper neck. This can be accompanied by nasal and laryngeal edema, which can cause serious adverse effects in recovery (see the recovery section below). Also, the Trendelenburg position causes a decrease in cerebral blood flow and an increase in intracranial pressure, which could potentially cause ischemia in low flow regions of the brain and/or the spinal cord (Brosnan et al. 2008).
Analgesia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


