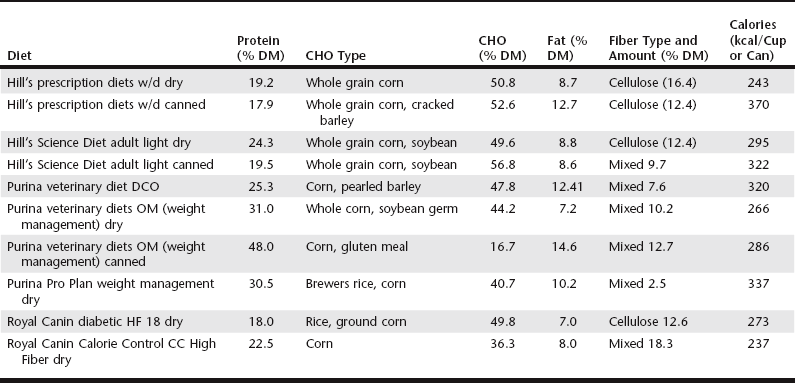
Chapter 46 Insulin therapy is the mainstay of treatment for both diabetic dogs and cats (see Chapters 44 and 48), but because diabetes is a disease of disordered metabolism, nutritional therapy is a key component of the management of these patients. Although different mechanisms for development of diabetes exist for dogs and cats, concurrent pancreatitis or other conditions (e.g., obesity) may be important factors for both species that influence the nutritional plan. The general goals of dietary therapy in any diabetic dog or cat are broad based and include the following: 1. To achieve and maintain optimal body condition 2. To provide a nutritionally complete, balanced, and palatable food that is readily consumed (so that intake is predictable) 3. To provide nutritional support for any concurrent diseases requiring nutritional modification 4. To maintain consistency in the timing and type (e.g., ingredients and calories) of food to assist in achieving optimal glycemic control 5. To control the amount and types of dietary starch, because the primary determinant of postprandial glycemia is starch, present in the diet. Finally, there is a highly variable difference between dogs in their response to dietary fiber—in other words, there does not appear to be a uniform effect of fiber in all diabetics, and the effect of a type or amount of fiber in a diabetic dog is unpredictable. An investigation in diabetic dogs comparing a canned, high-fiber, moderate-starch diet with a diet that contained a moderate amount of fiber and starch found no significant difference between the diets in insulin requirements or glycemic response. The decision to use a diet with increased dietary fiber in the therapy of a diabetic dog should be based on individual circumstances because there is no clear indication that these diets are beneficial in all cases. For example, in dogs that may need to lose weight or dogs with poor glycemic control with a normal maintenance diet, diets containing increased insoluble or mixed fiber may be a reasonable choice. Alternatively, if the dog does not tolerate or refuses to eat a diet with increased amounts of fiber, the clinician should choose a maintenance or weight-loss diet containing lower fat and high complex carbohydrates. Table 46-1 lists different diets, both fiber-containing veterinary diets and non–fiber-containing diets, that may be considered for use in diabetic dogs (this is not an exhaustive list). Diabetic dogs also have abnormalities in lipid metabolism secondary to the lack of insulin production, including hypertriglyceridemia; hypercholesterolemia; and increases in lipoproteins, chylomicrons, and free fatty acids. In contrast to humans, who have increased risk of cardiovascular disease and stroke secondary to hypertriglyceridemia, the major consequence in dogs is the increased risk of pancreatitis, which complicates the management of diabetes and increases the risk for secondary complications and morbidity (see Chapters 58 and 137). In most diabetic dogs, the lipid values improve with the administration of insulin and feeding a diet containing lower fat and higher fiber content. Current recommendations by nutritionists suggest feeding a diet that contains less than 30% of metabolizable energy from fat; however, there are very few published data on the influence of dietary fat or the optimal level of fat in dogs with diabetes.
Diet and Diabetes
Dietary Management of Canine Diabetes Mellitus
Dietary Fiber
Dietary Carbohydrates, Fat, and Protein
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree