CHAPTER 132 Ataxia
Ataxia, or incoordination of gait, is frequently associated with concurrent clinical signs of spasticity (stiffness) and paresis (weakness) and may be a result of diffuse disease or a focal or multifocal lesion anywhere in the central nervous system (CNS), including the cerebrum, cerebellum, brainstem, or spinal cord (Table 132-1). Cerebral, cerebellar, and brainstem lesions are uncommon but can result in ataxia in addition to other clinical signs referable to lesions in those areas. In this chapter, common conditions associated with ataxia are reviewed.
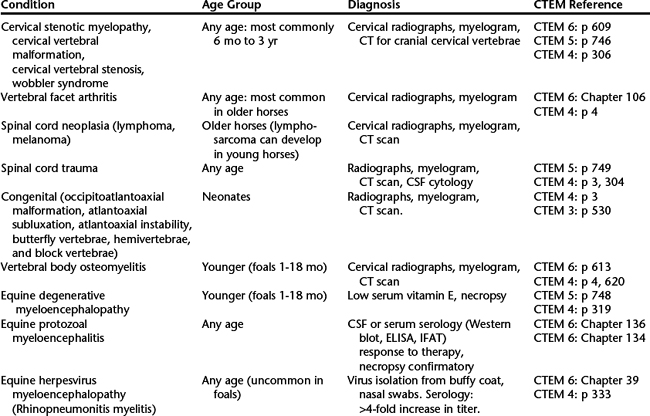
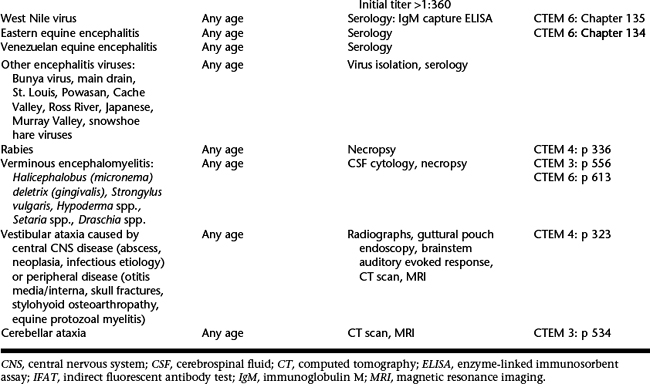
Table 132-1 Summary of Causes of Ataxia, Age of Affected Horses, Diagnostic Method, and Reference to This and Previous Editions of Current Therapy in Equine Medicine (CTEM)
CERVICAL VERTEBRAL STENOTIC MYELOPATHY
Bone malformation of the cervical vertebrae leads to narrowing of the cervical vertebral canal, which results in spinal cord compression and development of neurologic signs. CVSM can be divided into two forms: static and dynamic spinal cord compression. In horses with dynamic stenosis, compression of the spinal cord during a myelogram is observed only during movement of the neck, particularly during flexion (see Chapter 131, Diagnostic Imaging in Neurologic Disease). Dynamic compression primarily affects horses from 6 to 18 months of age and most commonly occurs at C3-4, followed in frequency by C4-5. During myelography, static cervical stenosis can be observed as a narrowing of the vertebral canal and resultant spinal cord compression at any neck position, although the compression is often exacerbated in the extended views of the neck. Static stenosis is most commonly observed at the C5-6 and C6-7 articulations in horses aged 1 to 4 years, but it is also seen in older horses. Horses older than 4 years often have clinically significant vertebral facet arthritis that can lead to further compression of the spinal cord, signs of neck pain, and even impingement on the spinal nerves as they exit the intervertebral foramina. This can lead to signs of lower motor neuron disease, including atrophy of cervical musculature, cutaneous hypalgesia, or focal sweating.



